Просмотров: 9 529
Systemic Scleroderma
Irina Alexandrovna Zborovskaya – doctor of medical sciences, professor,cathedral professor of hospital therapy with the course of clinical rheumatology of the doctors improvement faculty of Volgograd state medical university, director of the Federal Budgetary State Institution (FBSI) “Research and development institute of clinical and experimental rheumatology” of the RAMS, head of the regional Osteoporosis Center, presidium member of the Association of rheumatologists of Russia, member of the editorial boards of the magazines “Scientific and practical rheumatology” and “Modern rheumatology”
Definition. Scleroderma is a systemic disease of the connective tissue characterized by generalized degenerative and sclerotic changes of the connective tissue. Occlusion of the microvasculature (for example, Raynaud’s phenomenon), progressive fibrosis of skin and other tissues, including visceral organs, and angiospastic disturbances are common features of systemic scleroderma.

 In patients with CREST syndrome anticentromere antibodies are typically present. Internal organs are less commonly affected and the disease typically develops very slowly. Pulmonary fibrosis or primary biliary cirrhosis can occur even after several years of the disease. Systemic Raynaud`s phenomenon is also common. It is usually characterised by generalized vasoconstriction of arteries carrying blood to kidneys, heart and other organs.
Sclerodermia without scleroderma is the so-called visceral form of systemic scleroderma. In this case prognosis of the disease depends on the severity of the involvement of internal organs such as heart, lungs, kidneys.
Cross syndrome or mixed disease of the connective tissue is referred to as overlap-syndrome. Overlap syndrome is considered to be a rheumatic condition which is characterised by clinical manifestations of systemic scleroderma, rheumatoid arthritis, systemic lupus erythematosus and polymyositis. High-titred antibodies to ribonucleoproteins are typically present. This syndrome usually turns into systemic scleroderma or systemic lupus erythematosus.
Clinical manifestations. 95 percent of patients eventually develop skin involvement. Changes are typically present on the fingers and hands as well as on the proximal aspects of the trunk and face. Lower extremities are less commonly affected. The following phases are singled out in cutaneous changes: early (edematous) stage. Edema may appear thick or it may form a pit or erythema when pressing. Permeability of the walls of the vessels increases and endothelium of the small vessels is impaired. The early stage is followed by an indurated stage which is characterized by increased collagen synthesis. Atrophic stage is characterized by atrophy of the skin and its appendages, dryness of skin and connection of the skin with underlying tissues. Skin changes can lead to the changes of the face expression. The face becomes mask-like and amimic.
In patients with CREST syndrome anticentromere antibodies are typically present. Internal organs are less commonly affected and the disease typically develops very slowly. Pulmonary fibrosis or primary biliary cirrhosis can occur even after several years of the disease. Systemic Raynaud`s phenomenon is also common. It is usually characterised by generalized vasoconstriction of arteries carrying blood to kidneys, heart and other organs.
Sclerodermia without scleroderma is the so-called visceral form of systemic scleroderma. In this case prognosis of the disease depends on the severity of the involvement of internal organs such as heart, lungs, kidneys.
Cross syndrome or mixed disease of the connective tissue is referred to as overlap-syndrome. Overlap syndrome is considered to be a rheumatic condition which is characterised by clinical manifestations of systemic scleroderma, rheumatoid arthritis, systemic lupus erythematosus and polymyositis. High-titred antibodies to ribonucleoproteins are typically present. This syndrome usually turns into systemic scleroderma or systemic lupus erythematosus.
Clinical manifestations. 95 percent of patients eventually develop skin involvement. Changes are typically present on the fingers and hands as well as on the proximal aspects of the trunk and face. Lower extremities are less commonly affected. The following phases are singled out in cutaneous changes: early (edematous) stage. Edema may appear thick or it may form a pit or erythema when pressing. Permeability of the walls of the vessels increases and endothelium of the small vessels is impaired. The early stage is followed by an indurated stage which is characterized by increased collagen synthesis. Atrophic stage is characterized by atrophy of the skin and its appendages, dryness of skin and connection of the skin with underlying tissues. Skin changes can lead to the changes of the face expression. The face becomes mask-like and amimic.
 The nose and ears are thinned.
The nose and ears are thinned.
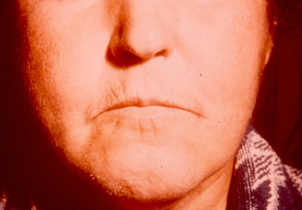 The mouth is narrowed and there are wrinkles at the angles of the mouth
The mouth is narrowed and there are wrinkles at the angles of the mouth
 The eyelids do not close fully.
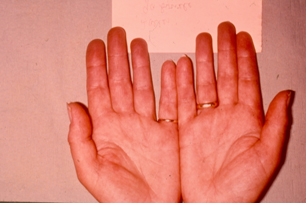
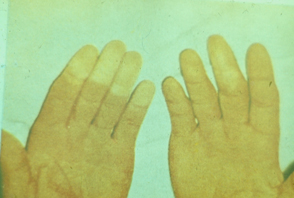
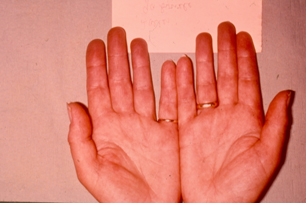
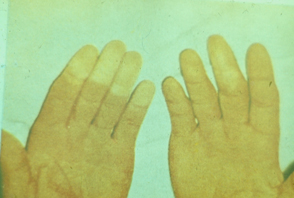
Changes of the hands are also common in systemic scleroderma.
The eyelids do not close fully.
Changes of the hands are also common in systemic scleroderma.
 They usually develop due to edema and induration. The fingers look like as if they are made of plaster cast.
They usually develop due to edema and induration. The fingers look like as if they are made of plaster cast.
 It is difficult to clench fists. Most patients usually develop osteolysis and shortening of phalanges.
It is difficult to clench fists. Most patients usually develop osteolysis and shortening of phalanges.
 As the disease progresses, most nail plates are dissolved.
Raynaud`s phenomenon develops in 95 percent of patients.
As the disease progresses, most nail plates are dissolved.
Raynaud`s phenomenon develops in 95 percent of patients.
 Raynaud`s phenomenon may precede obvious sclerodermatous features by months or even years. Symptoms may be not evident. Episodic spasms of the involved vessels of the fingers can cause colour changes of pallor (white), cyanosis (blue), and then redness (red) or reactive hyperemia.
Raynaud`s phenomenon may precede obvious sclerodermatous features by months or even years. Symptoms may be not evident. Episodic spasms of the involved vessels of the fingers can cause colour changes of pallor (white), cyanosis (blue), and then redness (red) or reactive hyperemia.
 Vasospastic disturbances in systemic scleroderma are typically noted in hands and feet. Sometimes numbness and whitening of lips, face, and the tip of the tongue may also occur.
Vasospastic disturbances can occur in internal organs (for example, in the brain, heart, lungs).
Telangiectasias typically develop in skin or/and in mucous membranes. Telangiectasias are referred to as star-shaped dilated capillaries and small vessels located just beneath the dermis on any skin area. 30 percent of patients develop telangiectasia in diffuse systemic scleroderma and 80% of patients develop telangiectasia in limited systemic scleroderma. Telangiectasias are more obvious at the advanced stage of the disease.
Subcutaneous calcinosis
Vasospastic disturbances in systemic scleroderma are typically noted in hands and feet. Sometimes numbness and whitening of lips, face, and the tip of the tongue may also occur.
Vasospastic disturbances can occur in internal organs (for example, in the brain, heart, lungs).
Telangiectasias typically develop in skin or/and in mucous membranes. Telangiectasias are referred to as star-shaped dilated capillaries and small vessels located just beneath the dermis on any skin area. 30 percent of patients develop telangiectasia in diffuse systemic scleroderma and 80% of patients develop telangiectasia in limited systemic scleroderma. Telangiectasias are more obvious at the advanced stage of the disease.
Subcutaneous calcinosis
 most commonly occurs on the fingers, elbows and knees; however, any area can be affected.
most commonly occurs on the fingers, elbows and knees; however, any area can be affected.
 For example, epiglottis, vocal cords, pericardium, valves and cardiac muscle, hepatic capsule and the capsule of the spleen can be affected.
For example, epiglottis, vocal cords, pericardium, valves and cardiac muscle, hepatic capsule and the capsule of the spleen can be affected.
 Skin ulceration often develops on the tips of the fingers due to impaired blood circulation.
Skin ulceration often develops on the tips of the fingers due to impaired blood circulation.
 Sometimes ulcerations may occur in the area of auricles and even eye-lids.
Gastrointestinal involvement occurs most commonly in systemic scleroderma. It is characterised by certain clinical and X-ray manifestations and it helps the doctor diagnose systemic scleroderma. Disorder of the motor function of the esophagus is typically due to atrophy of the smooth muscles and formation of collagen in the lower third of the esophagus.
Sometimes ulcerations may occur in the area of auricles and even eye-lids.
Gastrointestinal involvement occurs most commonly in systemic scleroderma. It is characterised by certain clinical and X-ray manifestations and it helps the doctor diagnose systemic scleroderma. Disorder of the motor function of the esophagus is typically due to atrophy of the smooth muscles and formation of collagen in the lower third of the esophagus.
 Esophageal sphincter incompetence is typically noted. Straited muscles of the upper third of the esophagus are not usually impaired. Reduced amplitude or absence of peristalsis of the lower third of the esophagus is commonly seen.
Esophageal sphincter incompetence is typically noted. Straited muscles of the upper third of the esophagus are not usually impaired. Reduced amplitude or absence of peristalsis of the lower third of the esophagus is commonly seen.
 It is often associated with gastroesophageal reflux disease which has the following symptoms: dysphagia, impaired swallowing, painful regurgitation, heartburn in the epigastrium and in the substernal area. Dysphagia (especially when swallowing) can occur without any other obvious symptoms of esophagus involvement. It is caused by decreased peristalsis of the esophagus due to neuromuscular disturbances.
According to the extent of severity of esophagus involvement, 3 degrees of sclerodermic involvement of the esophagus, which reflect the development of the pathologic process are singled out. They are the following:
1st degree – of moderate severity; it is characterized by a slightly slowed movement of barium sulfate from the cranial to the caudal parts of the esophagus.
2nd degree – clearly marked; it is characterized by a slowed movement of barium sulfate through the esophagus as well as prolonged delay of barium in the esophagus, opening, enlargement of the lumen of the esophagus, changes of the mucous membrane surface.
3rd degree – maximum; it is characterized by a slowed movement of barium sulfate through the esophagus and prolonged delay of barium sulfate in the esophagus, clearly marked enlargement of the lumen of the esophagus, changes of the mucous membrane surface, signs of gastroesophageal reflux disease and its secondary complications.
Esophagus ulcer most commonly occurs at the site of connection of the esophagus and the stomach. Sometimes it can cause bleeding from the esophagus. Along with this, gastroesophageal reflux disease can cause cylinder-cell metaplasia of the epithelium of the esophagus; however, adenocarcinoma develops quite rarely.
Enlargement, atony and slowed evacuation of the stomach are common features of stomach involvement. Changes occurring in the intestine are the same as in the esophagus. Sclerodermic duodenitis is clinically manifested by the disorder of the motor function of the intestine, cramps, diarrhea and pain. Malabsorption and syndrome of bacterial growth are common in small intestine involvement. Spue-like syndrome (that is weight loss, diarrhea and anemia) is also typical of small intestine involvement.
Severe constipation sometimes associated with partial recurrent intestinal obstruction and sacculation are typical of large intestine involvement. Telangiectasy of the stomach and intestine can cause gastrointestinal bleeding.
Mucous membrane involvement (as in Sjegren’s syndrome) is commonly noted in systemic scleroderma. Secretory insufficiency of exocrine glands develops due to a chronic inflammatory process in the glands. Enlarged parotid glands (fibrosis), dryness of mucous membranes of the eye (xerophthalmia) and that of the mouth (xerostomia), trachea, bronchi, stomach, vagina and skin are commonly noted in systemic scleroderma.
Endocrine glands are also commonly involved in systemic scleroderma. Hypothyroidism often develops due to chronic lymphocyte thyroiditis and fibrosis of the thyroid gland. Disorder of the function of the adrenal cortex, primary and secondary diabetes underlying interstitial fibrosis of the pancreas are typical of systemic scleroderma.
Articular syndrome is clinically manifested in 3 main forms. They are the following: polyarthralgia; sclerodermic polyarthritis associated with either exudative-proliferative or fibrous-indurative changes; and periarthritis associated with the development of fibrous contractures. Flexion contractures typically develop due to ligament involvement and progressive thickening/ of the skin.
It is often associated with gastroesophageal reflux disease which has the following symptoms: dysphagia, impaired swallowing, painful regurgitation, heartburn in the epigastrium and in the substernal area. Dysphagia (especially when swallowing) can occur without any other obvious symptoms of esophagus involvement. It is caused by decreased peristalsis of the esophagus due to neuromuscular disturbances.
According to the extent of severity of esophagus involvement, 3 degrees of sclerodermic involvement of the esophagus, which reflect the development of the pathologic process are singled out. They are the following:
1st degree – of moderate severity; it is characterized by a slightly slowed movement of barium sulfate from the cranial to the caudal parts of the esophagus.
2nd degree – clearly marked; it is characterized by a slowed movement of barium sulfate through the esophagus as well as prolonged delay of barium in the esophagus, opening, enlargement of the lumen of the esophagus, changes of the mucous membrane surface.
3rd degree – maximum; it is characterized by a slowed movement of barium sulfate through the esophagus and prolonged delay of barium sulfate in the esophagus, clearly marked enlargement of the lumen of the esophagus, changes of the mucous membrane surface, signs of gastroesophageal reflux disease and its secondary complications.
Esophagus ulcer most commonly occurs at the site of connection of the esophagus and the stomach. Sometimes it can cause bleeding from the esophagus. Along with this, gastroesophageal reflux disease can cause cylinder-cell metaplasia of the epithelium of the esophagus; however, adenocarcinoma develops quite rarely.
Enlargement, atony and slowed evacuation of the stomach are common features of stomach involvement. Changes occurring in the intestine are the same as in the esophagus. Sclerodermic duodenitis is clinically manifested by the disorder of the motor function of the intestine, cramps, diarrhea and pain. Malabsorption and syndrome of bacterial growth are common in small intestine involvement. Spue-like syndrome (that is weight loss, diarrhea and anemia) is also typical of small intestine involvement.
Severe constipation sometimes associated with partial recurrent intestinal obstruction and sacculation are typical of large intestine involvement. Telangiectasy of the stomach and intestine can cause gastrointestinal bleeding.
Mucous membrane involvement (as in Sjegren’s syndrome) is commonly noted in systemic scleroderma. Secretory insufficiency of exocrine glands develops due to a chronic inflammatory process in the glands. Enlarged parotid glands (fibrosis), dryness of mucous membranes of the eye (xerophthalmia) and that of the mouth (xerostomia), trachea, bronchi, stomach, vagina and skin are commonly noted in systemic scleroderma.
Endocrine glands are also commonly involved in systemic scleroderma. Hypothyroidism often develops due to chronic lymphocyte thyroiditis and fibrosis of the thyroid gland. Disorder of the function of the adrenal cortex, primary and secondary diabetes underlying interstitial fibrosis of the pancreas are typical of systemic scleroderma.
Articular syndrome is clinically manifested in 3 main forms. They are the following: polyarthralgia; sclerodermic polyarthritis associated with either exudative-proliferative or fibrous-indurative changes; and periarthritis associated with the development of fibrous contractures. Flexion contractures typically develop due to ligament involvement and progressive thickening/ of the skin.
 Some patients develop osteolysis (especially of the phalages).
Some patients develop osteolysis (especially of the phalages).
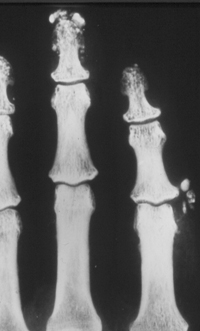 It is caused by vascular-trophic disturbances and is clinically manifested by shortening and deformity of the toes and fingers.
It is caused by vascular-trophic disturbances and is clinically manifested by shortening and deformity of the toes and fingers.
 Resorption of distal phalanges of the hands and feet, ribs, clavicles and the angle of the lower jaw may occur.
Resorption of distal phalanges of the hands and feet, ribs, clavicles and the angle of the lower jaw may occur.
 Osteolysis is not typically seen in other diseases of the connective tissue.
Muscle involvement in patients with systemic scleroderma is usually of mild severity. It is typically associated with a slight increase of enzyme activity and does not usually require any specific treatment. Sometimes fibrous interstitial myositis associated with atrophy of muscle fibers may occur. Patients may present with increased muscle weakness, less commonly myalgia.
Nervous system involvement is clinically manifested both by peripheral and central neuropathy.
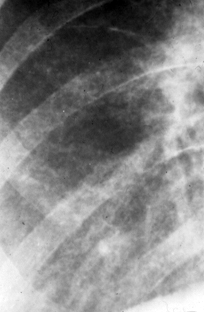
Pulmonary involvement in patients with systemic scleroderma includes: interstitial fibrosis or fibrosing alveolitis associated with the involvement of the lower lobes of the lungs; diffuse pulmonary fibrosis; involvement of the pulmonary vessels indicating the presence of pulmonary hypertension; pulmonary complications (viral and bacterial pneumonias, rupture of subpleural cysts associated with the development of pneumothorax, abscess formation, lung cancer associated with sclerodermic pneumofibrosis).
Osteolysis is not typically seen in other diseases of the connective tissue.
Muscle involvement in patients with systemic scleroderma is usually of mild severity. It is typically associated with a slight increase of enzyme activity and does not usually require any specific treatment. Sometimes fibrous interstitial myositis associated with atrophy of muscle fibers may occur. Patients may present with increased muscle weakness, less commonly myalgia.
Nervous system involvement is clinically manifested both by peripheral and central neuropathy.
Pulmonary involvement in patients with systemic scleroderma includes: interstitial fibrosis or fibrosing alveolitis associated with the involvement of the lower lobes of the lungs; diffuse pulmonary fibrosis; involvement of the pulmonary vessels indicating the presence of pulmonary hypertension; pulmonary complications (viral and bacterial pneumonias, rupture of subpleural cysts associated with the development of pneumothorax, abscess formation, lung cancer associated with sclerodermic pneumofibrosis).
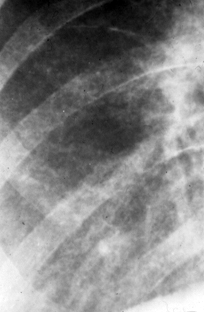 Pulmonary hypertension is clinically manifested by increased breathlessness resulting in the development of tricuspid insufficiency.
Survival rate in pulmonary hypertension averages 2 years. Bronchiectasis, emphysema, perifocal pneumonia, cystous pneumosclerosis typically occur in well pronounced pneumosclerosis. Pleurisy in systemic scleroderma is less common than in other rheumatic conditions.
Heart involvement includes changes of the myocardium, endocardium and pericardium.
Pulmonary hypertension is clinically manifested by increased breathlessness resulting in the development of tricuspid insufficiency.
Survival rate in pulmonary hypertension averages 2 years. Bronchiectasis, emphysema, perifocal pneumonia, cystous pneumosclerosis typically occur in well pronounced pneumosclerosis. Pleurisy in systemic scleroderma is less common than in other rheumatic conditions.
Heart involvement includes changes of the myocardium, endocardium and pericardium.
 At an early stage of myocardium involvement edema, inflammation and proliferation of a new loose connective tissue and sometimes areas of necrobiosis of muscle fibers can be noted.
Well pronounced myocardium involvement associated with cardiosclerosis, fibrous-sclerotic scarring of the cardiac muscle is referred to as myocardosis or interstitial myocarditis. Myocardial fibrosis with a large focus can indicate infarction-like changes on routine ECGs. However, in some cases it can lead to the development of “callous” heart aneurysm. Calcinosis of certain parts of the cardiac muscle may develop. Angina pectoris may occur in fibrous impairment of coronary arteries.
Endocardium involvement typically results in sclerodermic heart failure (that is calcinosis of the valves) which is characterized by a chronic course of the disease and sometimes by the development of decompensation. Mitral and tricuspid valves are most commonly affected.
Pericarditis as a manifestation of polyserositis has an adhesive-exudative character and is not clearly marked.
Renal involvement occurs in 80% of patients with systemic scleroderma and is characterized by the involvement of renal vessels. In true sclerodermic kidney progressive proteinuria, increased arterial blood pressure, oliguria, uremia, and terminal anuria are typically noted.
Sclerodermic renal crisis usually develops in the first 5 years after the onset of the disease. It typically occurs in patients with diffuse systemic scleroderma and presents as diffuse glomerulonephritis. Progressive oliguric acute renal insufficiency develops as a result of fibrosis of interlobular arteries associated with the effect of some vasoconstrictive stimuli such as diuresis, bleeding, surgical intervention.
Three degrees of chronic sclerodermic nephropathy are singled out. Minimum, subclinical chronic sclerodermic nephropathy is characterized by slight and unstable changes in urine and /or functional disturbances (reduction of glomerular filtration). Moderate chronic sclerodermic nephropathy is characterized by slight but stable changes in urine associated with dysfunction of kidneys.
In clearly marked chronic sclerodermic nephropathy patients develop hypertension, edema, hyperreninemia, urinary syndrome and functional disturbances.
Lab studies are usually non-specific and typically indicate the extent of disease activity and immune disturbances. Peripheral blood in systemic scleroderma does not change. However, some patients develop anemia, leukocytosis or (less commonly) leucopenia, increased ESR.
Increased fibrinogen, seromucoid, alfa-2-globuline, IgG may occur. Hyperproteinemia (hypergamma-globulinemia) may be also present.
Some autoantibodies can also be revealed in systemic scleroderma (Table 2). Rheumatoid factor may occur in 40 – 50 percent of patients, lupous LE-cells are present in 2 – 7 percent of patients, antinuclear factor is present in 60 – 70 percent of patients.
Table 2.
Autoantibodies revealed in systemic scleroderma
At an early stage of myocardium involvement edema, inflammation and proliferation of a new loose connective tissue and sometimes areas of necrobiosis of muscle fibers can be noted.
Well pronounced myocardium involvement associated with cardiosclerosis, fibrous-sclerotic scarring of the cardiac muscle is referred to as myocardosis or interstitial myocarditis. Myocardial fibrosis with a large focus can indicate infarction-like changes on routine ECGs. However, in some cases it can lead to the development of “callous” heart aneurysm. Calcinosis of certain parts of the cardiac muscle may develop. Angina pectoris may occur in fibrous impairment of coronary arteries.
Endocardium involvement typically results in sclerodermic heart failure (that is calcinosis of the valves) which is characterized by a chronic course of the disease and sometimes by the development of decompensation. Mitral and tricuspid valves are most commonly affected.
Pericarditis as a manifestation of polyserositis has an adhesive-exudative character and is not clearly marked.
Renal involvement occurs in 80% of patients with systemic scleroderma and is characterized by the involvement of renal vessels. In true sclerodermic kidney progressive proteinuria, increased arterial blood pressure, oliguria, uremia, and terminal anuria are typically noted.
Sclerodermic renal crisis usually develops in the first 5 years after the onset of the disease. It typically occurs in patients with diffuse systemic scleroderma and presents as diffuse glomerulonephritis. Progressive oliguric acute renal insufficiency develops as a result of fibrosis of interlobular arteries associated with the effect of some vasoconstrictive stimuli such as diuresis, bleeding, surgical intervention.
Three degrees of chronic sclerodermic nephropathy are singled out. Minimum, subclinical chronic sclerodermic nephropathy is characterized by slight and unstable changes in urine and /or functional disturbances (reduction of glomerular filtration). Moderate chronic sclerodermic nephropathy is characterized by slight but stable changes in urine associated with dysfunction of kidneys.
In clearly marked chronic sclerodermic nephropathy patients develop hypertension, edema, hyperreninemia, urinary syndrome and functional disturbances.
Lab studies are usually non-specific and typically indicate the extent of disease activity and immune disturbances. Peripheral blood in systemic scleroderma does not change. However, some patients develop anemia, leukocytosis or (less commonly) leucopenia, increased ESR.
Increased fibrinogen, seromucoid, alfa-2-globuline, IgG may occur. Hyperproteinemia (hypergamma-globulinemia) may be also present.
Some autoantibodies can also be revealed in systemic scleroderma (Table 2). Rheumatoid factor may occur in 40 – 50 percent of patients, lupous LE-cells are present in 2 – 7 percent of patients, antinuclear factor is present in 60 – 70 percent of patients.
Table 2.
Autoantibodies revealed in systemic scleroderma
Diagnostic criteria of systemic scleroderma (suggested by Guseva N.G., 1993)
Basic:
Peripheral:
1. Raynaud`s syndrome
2. Sclerodermic skin involvement
3. Articular-muscular syndrome (with contractures)
4. Osteolysis
5. Calcinosis
Visceral:
6. Basal pneumosclerosis
7. Cardiosclerosis with a large focus.
8. Sclerodermic gastrointestinal involvement
9. Acute sclerodermic nephropathy
Lab findings:
Specific AHA (anti-Scl-70 and anti-centromere antibodies)
Additional:
Peripheral:
1. Skin hyperemia
2. Telangiectasia
3. Trophic disturbances
4. Polyarthralgia
5. Polymyalgia, polymyositis
Visceral:
6. Lymphadenopathy
7. Polyserositis (most commonly adhesive)
8. Polyneuritis, central nervous system involvement
General:
1. Loss of body weight – more than 10 kg
2. Fever (most commonly subfebrile)
Lab findings:
1. Increased ESR (more than 20 mm/hr);
2. Hyperproteinemia (more than 75 g/l);
3. Hypergammaglobulinemia (more than 23%);
4. Antibodies to DNA or antinuclear factor;
5. Rheumatoid factor.
Differential diagnostics. Systemic scleroderma should be differentiated from other diseases of the connective tissue and conditions that have in common fibrosis of skin. Raynaud`s syndrome as well as some other vascular and visceral symptoms are not typical of many diseases of this group.
Systemic scleroderma should be differentiated from the following diseases:




Epidemiology. Scleroderma is found in all geographic locations and affects all races and ethnic groups worldwide. The incidence of scleroderma increases with age, reaching its peak in patients aged 30 – 40 years. The incidence for women is 3 times higher than for men. However, the incidence for women during childbearing years is 15 times higher than for men. The incidence of scleroderma averages 19 to 75 cases per 100,000 people.
Systemic scleroderma most commonly occurs in families, in persons carrying autoantibodies and those with increased prevalence of diseases of the connective tissue. Studies have shown that a higher risk exists for HLA-DR1, HLA-DR2, HLA-DR3, HLA-DR5, HLA-DQA2 carriers and C4A gene allele.
Aetiology. The exact aetiology of scleroderma is unclear. Environmental factors play a significant role in the development of systemic scleroderma. It was reported that a higher risk for developing systemic scleroderma exists for miners and builders who are exposed to silicon dust. Polyvinyl chloride exposure can also lead to the development of Raynaud`s syndrome, acroosteolysis, skin involvement and changes of the nail capillaries as well as to hepatic fibrosis and hemangiosarcoma. Exposure to epoxy resins and aromatic carbohydrates (for example, benzol and toluene) may also be a factor. Application of analgesics, such as pentazocine, can lead to pronounced fibrosis of skin and cell tissue. Administration of antitumor drugs, such as bleomycine, leads to the formation of fibrous nodes and hyperpigmentation of skin, alopecia, gangrene of fingers and pneumosclerosis. In pneumosclerosis the lower lobes of the lungs are usually the first to be involved.
Pathogenesis. The vessels of the endothelium are typically the first to be involved. At an early stage of systemic scleroderma intimal hyperplasia, typically present in sclerodermal vessels, can reduce the luminal diameter causing limited blood flow. Physiologic stimuli (for example, cold, emotions, thromboxane A2, serotonin) can increase the constriction of vessels and lead to the development of Raynaud` s phenomenon in skin and internal organs. Once kidneys are affected, stimulation of renin-angiotensin mechanism leads to the constriction of vessels.
At a later stage of the disease skin infiltration by activated T-lymphocytes, increased synthesis of IL-1, IL-4, IL-6 cytokines, proliferation of fibroblasts, synthesis of collagen Type 1 and 3 as well as release of platelet-derived growth factor and transforming growth factor-beta can be noted. Activation of mast cells leads to triptase synthesis which activates transforming growth factor-β. It also contributes to the production of eosinophilic cation protein and histamine which stimulates proliferation of fibroblasts and synthesis of matrix components. Development of Raynaud`s phenomenon is accounted for by complex immunologic interactions of endothelial (for example, nitrogen oxide, endothelin-1, prostaglandins) and platelet mediators (such as serotonin, beta-thromboglobulin) as well as neuropeptides such as peptide associated with calcitonin and vasoactive intestinal polypeptide.
Endothelium involvement and insufficiency of tissue-type plasminogen activator contribute to intravascular coagulation and in severe cases can cause hemolytic microangiopathic anemia.
Skin biopsy near the foci of sclerosis demonstrates perivascular and diffuse skin infiltration caused by T-lymphocytes and macrophages. T-lymphocytes are typically represented by T-helpers. Increased level of IL-2 cytokines, IL-2 free receptors, CD4 free molecules as well as activation of adenosine deaminase in blood serum of patients indicate activation of T-helpers. Basal membranes of vessels can be a target for cellular immune reactions which occur in this condition. Adhesion molecules contributing to interaction of T-lymphocytes with endothelium play a role in the pathogenesis of systemic scleroderma.
In healthy people collagen Type VII is considered to be the main component of attachment fibrils which stabilize the link between epidermis and derma. In patients with systemic scleroderma collagen Type VII is found in the derma. That’s why the skin is thickened and connected with underlying tissues.
Humoral immunity is typically impaired in patients with systemic scleroderma. 95 percent of patients have antinuclear antibodies in blood serum. Some patients have antibodies to laminin and collagen Type IV. However, the significance of auto-antibodies in pathogenesis of the disease is unclear.
Classification of systemic scleroderma is presented in Table 1.
Acute, subacute and chronic courses of the disease are typically singled out. In an acute course of the disease systemic scleroderma is characterized by rapid progression of both skin and internal organ lesions. Progressive renal failure, especially in the first years after the onset of the disease, typically leads to death. In a subacute course of the disease systemic scleroderma is characterised by a gradual onset. In this case skin is usually involved. It is typically associated with sclerodermatous edema and skin induration, recurrent polyarthritis, myositis with myasthenic syndrome, involvement of internal organs. Cross syndromes can also be noted. In a chronic course of the disease systemic scleroderma is characterized by progressive vasomotor disturbances such as Raynaud`s syndrome, and clearly marked trophic disturbances which may be the only finding for many years and which further typically prevail in clinical presentation.
Skin and para-articular tissues become thickened leading to the development of contractures and osteolysis. Slow- progressing sclerotic changes of internal organs are also common in systemic scleroderma.
Table 1.
Classification of systemic scleroderma (suggested by Guseva N.G.,1994)
According to the disease activity, maximum (3rd degree), moderate (2nd degree) and minimum (1st degree) degree of disease activity are singled out.
According to the extent of disease progression, the stage of initial clinical manifestations (for example, Raynaud`s syndrome, polyarthralgia, arthritis, and less commonly skin, visceral or general manifestations), generalized or diffuse stage (characterised by numerous clinical manifestations) and terminal stage of the disease are singled out. Terminal stage is typically characterized by sclerotic, dystrophic and vascular-necrotic changes of organs associated with the disorder of their function.
The following main clinical forms of systemic scleroderma are singled out:
| Course of the disease | Stage of development | Extent of disease activity | Clinical and morphologic characteristics of changes occurring in systemic scleroderma | ||||||
| Skin and peripheral vessels | Musculo-skeletal system | Heart | Lungs | Gastro-intestinal tract | Kidneys | Nervous system | |||
| Acute Subacute Chronic | I – initial II – generalized III – terminal | I (minimum) II (moderate) III (maximum) | Thickened and indurated edema, atrophy, hyperpigmen- tation, telangiectasy, Raynaud’s syndrome, focal lesions. | Arthralgia, polyarthritis (exudative or fibrous-indurative, pseudoarthri-tis, polymyositis, calcinosis, osteolysis. | Myocardosis, cardiosclero-sis, heart failure (insufficiency of mitral valve – most commonly). | Interstitial pneumonia, pneumoscle-rosis (compact or cystous), adhisive pleurisy. | Esophagitis, duodenitis, colitis, spreu-like syndrome. | True scleroder-mic kidney, chronic diffuse nephritis, focal nephritis. | Polyneuritis, neuropsychic disturbances, vegetative shifts. |
| Clinical forms I. Typical (associated with common skin lesions); II. Atypical forms: With focal lesion of skin; Predominantly visceral; Articular; Muscular; Vascular. | |||||||||
- Prescleroderma
- Diffuse skin sclerodema
- Limited skin scleroderma
- Sclerodermia without scleroderma
- Cross-syndrome
 In patients with CREST syndrome anticentromere antibodies are typically present. Internal organs are less commonly affected and the disease typically develops very slowly. Pulmonary fibrosis or primary biliary cirrhosis can occur even after several years of the disease. Systemic Raynaud`s phenomenon is also common. It is usually characterised by generalized vasoconstriction of arteries carrying blood to kidneys, heart and other organs.
Sclerodermia without scleroderma is the so-called visceral form of systemic scleroderma. In this case prognosis of the disease depends on the severity of the involvement of internal organs such as heart, lungs, kidneys.
Cross syndrome or mixed disease of the connective tissue is referred to as overlap-syndrome. Overlap syndrome is considered to be a rheumatic condition which is characterised by clinical manifestations of systemic scleroderma, rheumatoid arthritis, systemic lupus erythematosus and polymyositis. High-titred antibodies to ribonucleoproteins are typically present. This syndrome usually turns into systemic scleroderma or systemic lupus erythematosus.
Clinical manifestations. 95 percent of patients eventually develop skin involvement. Changes are typically present on the fingers and hands as well as on the proximal aspects of the trunk and face. Lower extremities are less commonly affected. The following phases are singled out in cutaneous changes: early (edematous) stage. Edema may appear thick or it may form a pit or erythema when pressing. Permeability of the walls of the vessels increases and endothelium of the small vessels is impaired. The early stage is followed by an indurated stage which is characterized by increased collagen synthesis. Atrophic stage is characterized by atrophy of the skin and its appendages, dryness of skin and connection of the skin with underlying tissues. Skin changes can lead to the changes of the face expression. The face becomes mask-like and amimic.
In patients with CREST syndrome anticentromere antibodies are typically present. Internal organs are less commonly affected and the disease typically develops very slowly. Pulmonary fibrosis or primary biliary cirrhosis can occur even after several years of the disease. Systemic Raynaud`s phenomenon is also common. It is usually characterised by generalized vasoconstriction of arteries carrying blood to kidneys, heart and other organs.
Sclerodermia without scleroderma is the so-called visceral form of systemic scleroderma. In this case prognosis of the disease depends on the severity of the involvement of internal organs such as heart, lungs, kidneys.
Cross syndrome or mixed disease of the connective tissue is referred to as overlap-syndrome. Overlap syndrome is considered to be a rheumatic condition which is characterised by clinical manifestations of systemic scleroderma, rheumatoid arthritis, systemic lupus erythematosus and polymyositis. High-titred antibodies to ribonucleoproteins are typically present. This syndrome usually turns into systemic scleroderma or systemic lupus erythematosus.
Clinical manifestations. 95 percent of patients eventually develop skin involvement. Changes are typically present on the fingers and hands as well as on the proximal aspects of the trunk and face. Lower extremities are less commonly affected. The following phases are singled out in cutaneous changes: early (edematous) stage. Edema may appear thick or it may form a pit or erythema when pressing. Permeability of the walls of the vessels increases and endothelium of the small vessels is impaired. The early stage is followed by an indurated stage which is characterized by increased collagen synthesis. Atrophic stage is characterized by atrophy of the skin and its appendages, dryness of skin and connection of the skin with underlying tissues. Skin changes can lead to the changes of the face expression. The face becomes mask-like and amimic.
 The nose and ears are thinned.
The nose and ears are thinned.
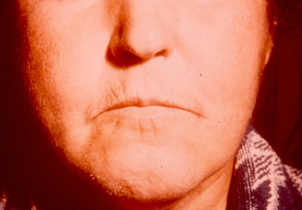 The mouth is narrowed and there are wrinkles at the angles of the mouth
The mouth is narrowed and there are wrinkles at the angles of the mouth
 The eyelids do not close fully.
Changes of the hands are also common in systemic scleroderma.
The eyelids do not close fully.
Changes of the hands are also common in systemic scleroderma.
 They usually develop due to edema and induration. The fingers look like as if they are made of plaster cast.
They usually develop due to edema and induration. The fingers look like as if they are made of plaster cast.
 It is difficult to clench fists. Most patients usually develop osteolysis and shortening of phalanges.
It is difficult to clench fists. Most patients usually develop osteolysis and shortening of phalanges.
 As the disease progresses, most nail plates are dissolved.
Raynaud`s phenomenon develops in 95 percent of patients.
As the disease progresses, most nail plates are dissolved.
Raynaud`s phenomenon develops in 95 percent of patients.
 Raynaud`s phenomenon may precede obvious sclerodermatous features by months or even years. Symptoms may be not evident. Episodic spasms of the involved vessels of the fingers can cause colour changes of pallor (white), cyanosis (blue), and then redness (red) or reactive hyperemia.
Raynaud`s phenomenon may precede obvious sclerodermatous features by months or even years. Symptoms may be not evident. Episodic spasms of the involved vessels of the fingers can cause colour changes of pallor (white), cyanosis (blue), and then redness (red) or reactive hyperemia.
 Vasospastic disturbances in systemic scleroderma are typically noted in hands and feet. Sometimes numbness and whitening of lips, face, and the tip of the tongue may also occur.
Vasospastic disturbances can occur in internal organs (for example, in the brain, heart, lungs).
Telangiectasias typically develop in skin or/and in mucous membranes. Telangiectasias are referred to as star-shaped dilated capillaries and small vessels located just beneath the dermis on any skin area. 30 percent of patients develop telangiectasia in diffuse systemic scleroderma and 80% of patients develop telangiectasia in limited systemic scleroderma. Telangiectasias are more obvious at the advanced stage of the disease.
Subcutaneous calcinosis
Vasospastic disturbances in systemic scleroderma are typically noted in hands and feet. Sometimes numbness and whitening of lips, face, and the tip of the tongue may also occur.
Vasospastic disturbances can occur in internal organs (for example, in the brain, heart, lungs).
Telangiectasias typically develop in skin or/and in mucous membranes. Telangiectasias are referred to as star-shaped dilated capillaries and small vessels located just beneath the dermis on any skin area. 30 percent of patients develop telangiectasia in diffuse systemic scleroderma and 80% of patients develop telangiectasia in limited systemic scleroderma. Telangiectasias are more obvious at the advanced stage of the disease.
Subcutaneous calcinosis
 most commonly occurs on the fingers, elbows and knees; however, any area can be affected.
most commonly occurs on the fingers, elbows and knees; however, any area can be affected.
 For example, epiglottis, vocal cords, pericardium, valves and cardiac muscle, hepatic capsule and the capsule of the spleen can be affected.
For example, epiglottis, vocal cords, pericardium, valves and cardiac muscle, hepatic capsule and the capsule of the spleen can be affected.
 Skin ulceration often develops on the tips of the fingers due to impaired blood circulation.
Skin ulceration often develops on the tips of the fingers due to impaired blood circulation.
 Sometimes ulcerations may occur in the area of auricles and even eye-lids.
Gastrointestinal involvement occurs most commonly in systemic scleroderma. It is characterised by certain clinical and X-ray manifestations and it helps the doctor diagnose systemic scleroderma. Disorder of the motor function of the esophagus is typically due to atrophy of the smooth muscles and formation of collagen in the lower third of the esophagus.
Sometimes ulcerations may occur in the area of auricles and even eye-lids.
Gastrointestinal involvement occurs most commonly in systemic scleroderma. It is characterised by certain clinical and X-ray manifestations and it helps the doctor diagnose systemic scleroderma. Disorder of the motor function of the esophagus is typically due to atrophy of the smooth muscles and formation of collagen in the lower third of the esophagus.
 Esophageal sphincter incompetence is typically noted. Straited muscles of the upper third of the esophagus are not usually impaired. Reduced amplitude or absence of peristalsis of the lower third of the esophagus is commonly seen.
Esophageal sphincter incompetence is typically noted. Straited muscles of the upper third of the esophagus are not usually impaired. Reduced amplitude or absence of peristalsis of the lower third of the esophagus is commonly seen.
 It is often associated with gastroesophageal reflux disease which has the following symptoms: dysphagia, impaired swallowing, painful regurgitation, heartburn in the epigastrium and in the substernal area. Dysphagia (especially when swallowing) can occur without any other obvious symptoms of esophagus involvement. It is caused by decreased peristalsis of the esophagus due to neuromuscular disturbances.
According to the extent of severity of esophagus involvement, 3 degrees of sclerodermic involvement of the esophagus, which reflect the development of the pathologic process are singled out. They are the following:
1st degree – of moderate severity; it is characterized by a slightly slowed movement of barium sulfate from the cranial to the caudal parts of the esophagus.
2nd degree – clearly marked; it is characterized by a slowed movement of barium sulfate through the esophagus as well as prolonged delay of barium in the esophagus, opening, enlargement of the lumen of the esophagus, changes of the mucous membrane surface.
3rd degree – maximum; it is characterized by a slowed movement of barium sulfate through the esophagus and prolonged delay of barium sulfate in the esophagus, clearly marked enlargement of the lumen of the esophagus, changes of the mucous membrane surface, signs of gastroesophageal reflux disease and its secondary complications.
Esophagus ulcer most commonly occurs at the site of connection of the esophagus and the stomach. Sometimes it can cause bleeding from the esophagus. Along with this, gastroesophageal reflux disease can cause cylinder-cell metaplasia of the epithelium of the esophagus; however, adenocarcinoma develops quite rarely.
Enlargement, atony and slowed evacuation of the stomach are common features of stomach involvement. Changes occurring in the intestine are the same as in the esophagus. Sclerodermic duodenitis is clinically manifested by the disorder of the motor function of the intestine, cramps, diarrhea and pain. Malabsorption and syndrome of bacterial growth are common in small intestine involvement. Spue-like syndrome (that is weight loss, diarrhea and anemia) is also typical of small intestine involvement.
Severe constipation sometimes associated with partial recurrent intestinal obstruction and sacculation are typical of large intestine involvement. Telangiectasy of the stomach and intestine can cause gastrointestinal bleeding.
Mucous membrane involvement (as in Sjegren’s syndrome) is commonly noted in systemic scleroderma. Secretory insufficiency of exocrine glands develops due to a chronic inflammatory process in the glands. Enlarged parotid glands (fibrosis), dryness of mucous membranes of the eye (xerophthalmia) and that of the mouth (xerostomia), trachea, bronchi, stomach, vagina and skin are commonly noted in systemic scleroderma.
Endocrine glands are also commonly involved in systemic scleroderma. Hypothyroidism often develops due to chronic lymphocyte thyroiditis and fibrosis of the thyroid gland. Disorder of the function of the adrenal cortex, primary and secondary diabetes underlying interstitial fibrosis of the pancreas are typical of systemic scleroderma.
Articular syndrome is clinically manifested in 3 main forms. They are the following: polyarthralgia; sclerodermic polyarthritis associated with either exudative-proliferative or fibrous-indurative changes; and periarthritis associated with the development of fibrous contractures. Flexion contractures typically develop due to ligament involvement and progressive thickening/ of the skin.
It is often associated with gastroesophageal reflux disease which has the following symptoms: dysphagia, impaired swallowing, painful regurgitation, heartburn in the epigastrium and in the substernal area. Dysphagia (especially when swallowing) can occur without any other obvious symptoms of esophagus involvement. It is caused by decreased peristalsis of the esophagus due to neuromuscular disturbances.
According to the extent of severity of esophagus involvement, 3 degrees of sclerodermic involvement of the esophagus, which reflect the development of the pathologic process are singled out. They are the following:
1st degree – of moderate severity; it is characterized by a slightly slowed movement of barium sulfate from the cranial to the caudal parts of the esophagus.
2nd degree – clearly marked; it is characterized by a slowed movement of barium sulfate through the esophagus as well as prolonged delay of barium in the esophagus, opening, enlargement of the lumen of the esophagus, changes of the mucous membrane surface.
3rd degree – maximum; it is characterized by a slowed movement of barium sulfate through the esophagus and prolonged delay of barium sulfate in the esophagus, clearly marked enlargement of the lumen of the esophagus, changes of the mucous membrane surface, signs of gastroesophageal reflux disease and its secondary complications.
Esophagus ulcer most commonly occurs at the site of connection of the esophagus and the stomach. Sometimes it can cause bleeding from the esophagus. Along with this, gastroesophageal reflux disease can cause cylinder-cell metaplasia of the epithelium of the esophagus; however, adenocarcinoma develops quite rarely.
Enlargement, atony and slowed evacuation of the stomach are common features of stomach involvement. Changes occurring in the intestine are the same as in the esophagus. Sclerodermic duodenitis is clinically manifested by the disorder of the motor function of the intestine, cramps, diarrhea and pain. Malabsorption and syndrome of bacterial growth are common in small intestine involvement. Spue-like syndrome (that is weight loss, diarrhea and anemia) is also typical of small intestine involvement.
Severe constipation sometimes associated with partial recurrent intestinal obstruction and sacculation are typical of large intestine involvement. Telangiectasy of the stomach and intestine can cause gastrointestinal bleeding.
Mucous membrane involvement (as in Sjegren’s syndrome) is commonly noted in systemic scleroderma. Secretory insufficiency of exocrine glands develops due to a chronic inflammatory process in the glands. Enlarged parotid glands (fibrosis), dryness of mucous membranes of the eye (xerophthalmia) and that of the mouth (xerostomia), trachea, bronchi, stomach, vagina and skin are commonly noted in systemic scleroderma.
Endocrine glands are also commonly involved in systemic scleroderma. Hypothyroidism often develops due to chronic lymphocyte thyroiditis and fibrosis of the thyroid gland. Disorder of the function of the adrenal cortex, primary and secondary diabetes underlying interstitial fibrosis of the pancreas are typical of systemic scleroderma.
Articular syndrome is clinically manifested in 3 main forms. They are the following: polyarthralgia; sclerodermic polyarthritis associated with either exudative-proliferative or fibrous-indurative changes; and periarthritis associated with the development of fibrous contractures. Flexion contractures typically develop due to ligament involvement and progressive thickening/ of the skin.
 Some patients develop osteolysis (especially of the phalages).
Some patients develop osteolysis (especially of the phalages).
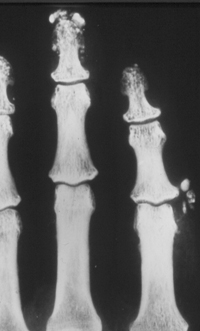 It is caused by vascular-trophic disturbances and is clinically manifested by shortening and deformity of the toes and fingers.
It is caused by vascular-trophic disturbances and is clinically manifested by shortening and deformity of the toes and fingers.
 Resorption of distal phalanges of the hands and feet, ribs, clavicles and the angle of the lower jaw may occur.
Resorption of distal phalanges of the hands and feet, ribs, clavicles and the angle of the lower jaw may occur.
 Osteolysis is not typically seen in other diseases of the connective tissue.
Muscle involvement in patients with systemic scleroderma is usually of mild severity. It is typically associated with a slight increase of enzyme activity and does not usually require any specific treatment. Sometimes fibrous interstitial myositis associated with atrophy of muscle fibers may occur. Patients may present with increased muscle weakness, less commonly myalgia.
Nervous system involvement is clinically manifested both by peripheral and central neuropathy.
Pulmonary involvement in patients with systemic scleroderma includes: interstitial fibrosis or fibrosing alveolitis associated with the involvement of the lower lobes of the lungs; diffuse pulmonary fibrosis; involvement of the pulmonary vessels indicating the presence of pulmonary hypertension; pulmonary complications (viral and bacterial pneumonias, rupture of subpleural cysts associated with the development of pneumothorax, abscess formation, lung cancer associated with sclerodermic pneumofibrosis).
Osteolysis is not typically seen in other diseases of the connective tissue.
Muscle involvement in patients with systemic scleroderma is usually of mild severity. It is typically associated with a slight increase of enzyme activity and does not usually require any specific treatment. Sometimes fibrous interstitial myositis associated with atrophy of muscle fibers may occur. Patients may present with increased muscle weakness, less commonly myalgia.
Nervous system involvement is clinically manifested both by peripheral and central neuropathy.
Pulmonary involvement in patients with systemic scleroderma includes: interstitial fibrosis or fibrosing alveolitis associated with the involvement of the lower lobes of the lungs; diffuse pulmonary fibrosis; involvement of the pulmonary vessels indicating the presence of pulmonary hypertension; pulmonary complications (viral and bacterial pneumonias, rupture of subpleural cysts associated with the development of pneumothorax, abscess formation, lung cancer associated with sclerodermic pneumofibrosis).
 Pulmonary hypertension is clinically manifested by increased breathlessness resulting in the development of tricuspid insufficiency.
Survival rate in pulmonary hypertension averages 2 years. Bronchiectasis, emphysema, perifocal pneumonia, cystous pneumosclerosis typically occur in well pronounced pneumosclerosis. Pleurisy in systemic scleroderma is less common than in other rheumatic conditions.
Heart involvement includes changes of the myocardium, endocardium and pericardium.
Pulmonary hypertension is clinically manifested by increased breathlessness resulting in the development of tricuspid insufficiency.
Survival rate in pulmonary hypertension averages 2 years. Bronchiectasis, emphysema, perifocal pneumonia, cystous pneumosclerosis typically occur in well pronounced pneumosclerosis. Pleurisy in systemic scleroderma is less common than in other rheumatic conditions.
Heart involvement includes changes of the myocardium, endocardium and pericardium.
 At an early stage of myocardium involvement edema, inflammation and proliferation of a new loose connective tissue and sometimes areas of necrobiosis of muscle fibers can be noted.
Well pronounced myocardium involvement associated with cardiosclerosis, fibrous-sclerotic scarring of the cardiac muscle is referred to as myocardosis or interstitial myocarditis. Myocardial fibrosis with a large focus can indicate infarction-like changes on routine ECGs. However, in some cases it can lead to the development of “callous” heart aneurysm. Calcinosis of certain parts of the cardiac muscle may develop. Angina pectoris may occur in fibrous impairment of coronary arteries.
Endocardium involvement typically results in sclerodermic heart failure (that is calcinosis of the valves) which is characterized by a chronic course of the disease and sometimes by the development of decompensation. Mitral and tricuspid valves are most commonly affected.
Pericarditis as a manifestation of polyserositis has an adhesive-exudative character and is not clearly marked.
Renal involvement occurs in 80% of patients with systemic scleroderma and is characterized by the involvement of renal vessels. In true sclerodermic kidney progressive proteinuria, increased arterial blood pressure, oliguria, uremia, and terminal anuria are typically noted.
Sclerodermic renal crisis usually develops in the first 5 years after the onset of the disease. It typically occurs in patients with diffuse systemic scleroderma and presents as diffuse glomerulonephritis. Progressive oliguric acute renal insufficiency develops as a result of fibrosis of interlobular arteries associated with the effect of some vasoconstrictive stimuli such as diuresis, bleeding, surgical intervention.
Three degrees of chronic sclerodermic nephropathy are singled out. Minimum, subclinical chronic sclerodermic nephropathy is characterized by slight and unstable changes in urine and /or functional disturbances (reduction of glomerular filtration). Moderate chronic sclerodermic nephropathy is characterized by slight but stable changes in urine associated with dysfunction of kidneys.
In clearly marked chronic sclerodermic nephropathy patients develop hypertension, edema, hyperreninemia, urinary syndrome and functional disturbances.
Lab studies are usually non-specific and typically indicate the extent of disease activity and immune disturbances. Peripheral blood in systemic scleroderma does not change. However, some patients develop anemia, leukocytosis or (less commonly) leucopenia, increased ESR.
Increased fibrinogen, seromucoid, alfa-2-globuline, IgG may occur. Hyperproteinemia (hypergamma-globulinemia) may be also present.
Some autoantibodies can also be revealed in systemic scleroderma (Table 2). Rheumatoid factor may occur in 40 – 50 percent of patients, lupous LE-cells are present in 2 – 7 percent of patients, antinuclear factor is present in 60 – 70 percent of patients.
Table 2.
Autoantibodies revealed in systemic scleroderma
At an early stage of myocardium involvement edema, inflammation and proliferation of a new loose connective tissue and sometimes areas of necrobiosis of muscle fibers can be noted.
Well pronounced myocardium involvement associated with cardiosclerosis, fibrous-sclerotic scarring of the cardiac muscle is referred to as myocardosis or interstitial myocarditis. Myocardial fibrosis with a large focus can indicate infarction-like changes on routine ECGs. However, in some cases it can lead to the development of “callous” heart aneurysm. Calcinosis of certain parts of the cardiac muscle may develop. Angina pectoris may occur in fibrous impairment of coronary arteries.
Endocardium involvement typically results in sclerodermic heart failure (that is calcinosis of the valves) which is characterized by a chronic course of the disease and sometimes by the development of decompensation. Mitral and tricuspid valves are most commonly affected.
Pericarditis as a manifestation of polyserositis has an adhesive-exudative character and is not clearly marked.
Renal involvement occurs in 80% of patients with systemic scleroderma and is characterized by the involvement of renal vessels. In true sclerodermic kidney progressive proteinuria, increased arterial blood pressure, oliguria, uremia, and terminal anuria are typically noted.
Sclerodermic renal crisis usually develops in the first 5 years after the onset of the disease. It typically occurs in patients with diffuse systemic scleroderma and presents as diffuse glomerulonephritis. Progressive oliguric acute renal insufficiency develops as a result of fibrosis of interlobular arteries associated with the effect of some vasoconstrictive stimuli such as diuresis, bleeding, surgical intervention.
Three degrees of chronic sclerodermic nephropathy are singled out. Minimum, subclinical chronic sclerodermic nephropathy is characterized by slight and unstable changes in urine and /or functional disturbances (reduction of glomerular filtration). Moderate chronic sclerodermic nephropathy is characterized by slight but stable changes in urine associated with dysfunction of kidneys.
In clearly marked chronic sclerodermic nephropathy patients develop hypertension, edema, hyperreninemia, urinary syndrome and functional disturbances.
Lab studies are usually non-specific and typically indicate the extent of disease activity and immune disturbances. Peripheral blood in systemic scleroderma does not change. However, some patients develop anemia, leukocytosis or (less commonly) leucopenia, increased ESR.
Increased fibrinogen, seromucoid, alfa-2-globuline, IgG may occur. Hyperproteinemia (hypergamma-globulinemia) may be also present.
Some autoantibodies can also be revealed in systemic scleroderma (Table 2). Rheumatoid factor may occur in 40 – 50 percent of patients, lupous LE-cells are present in 2 – 7 percent of patients, antinuclear factor is present in 60 – 70 percent of patients.
Table 2.
Autoantibodies revealed in systemic scleroderma
| Autoantibodies | Type of disease | Detection rate, % |
| Antibodies to Scl-70 antigene | Diffuse | 40 |
| Antibodies to centromeres | Limited | 60-80 |
| Antibodies to RNA-polymerase I, II, III | Diffuse | 5-40 |
| Antibodies to Th-ribonucleoproteid | Limited | 14 |
| Limited | 5-10 | |
| Mixed disease of the connective tissue | 95-100 | |
| Antibodies to PM-1 antigen | Cross-syndrome associated with clinical manifestations of polymyositis and limited type of systemic scleroderma | 25 |
- Rheumatoid arthritis
- Polymyositis (dermatomiositis) and antisynthetase syndrome
- Vasculitis (thromboangiitis obliterans, arteritis Takayasu); atherosclerosis
- Systemic lupus erythematosus
- Primary Sjegren’s sicca syndrome
- Mixed diseases of the connective tissue
- Diseases associated with increased blood viscosity (cryoglobulinemia, polycithemia, Waldenstrem`s macroglobulinemia)
- Tunnel syndromes
- Endocrine diseases
- Prevention and treatment of vascular complications
- Control of fibrosis progression
- Effecting the main immuno-inflammatory mechanisms of systemic scleroderma
- Prevention and treatment of internal organ involvement
- High activity of sclerodermic process
- Well pronounced immune shifts