Просмотров: 9 876
Bechterew’s (Strumpell-Marie) Disease or Ankylosing Spondylitis
Irina Alexandrovna Zborovskaya – doctor of medical sciences, professor, head of the department of hospital therapy with the course of clinical rheumatology of the doctors improvement faculty of Volgograd state medical university, deputy director for scientific work of the State institution “Research and development institute of clinical and experimental rheumatology” of the RAMS, head of the regional Osteoporosis Center, presidium member of the Association of rheumatologists of Russia, member of the editorial boards of the magazines “Scientific and practical rheumatology” and “Modern rheumatology”
Definition. Bechterew’s disease or ankylosing spondylitis is a member of a group of rheumatic diseases that affects the spinal column known as “seronegative spondylarthritis”. Ankylosing spondylitis is a chronic, inflammatory rheumatic disease that causes inflammation of the spinal joints (vertebrae), perivertebral tissues and sacroiliac joint. The chronic inflammation of vertebrae can eventually cause ankylosis of intervertebral joints and calcification of spinal ligaments.
Epidemiology. The incidence of ankylosing spondylitis has been estimated 1:1000 (one case per thousand people). Prevalence of ankylosing spondylitis parallels the prevalence of HLA-B27 gene in the general population and prevalence of ankylosing spondylitis in certain geographic locations. HLA-B27 antigen occurs in 7% of white Americans and in 90% of individuals with ankylosing spondylitis. The gene which codes HLA-B27 antigen is found in chromosome 6. HLA-B27 antigen does not effect the extent of the disease severity.
Sex. Ankylosing spondylitis occurs as frequently in men as in women considering sacroileitis as a diagnostic criterion of the disease. However, symptoms of the disease are generally milder among females. Peripheral joints are most commonly involved in females than in males.
Genetic predisposition. Families of patients with HLA-B27 antigen have a higher disease incidence which amounts to 20% of all cases. Concordance rate of ankylosing spondylitis among monozygotic twins is about 50%. These findings testify to the fact that not only HLA-B27 antigen but also some other genes and environmental factors play a significant role in pathogenesis of ankylosing spondylitis.
Aetiology. The exact cause of ankylosing spondylitis remains unknown. However, it has been demonstrated that ankylosing spondylitis tends to run in families. A specific HLA-B27 histocompatibility antigen occurring in 90-95% of individuals is also of great importance. Infections may be also a factor. There is evidence for a possible role of Klebsiella and some other species in the development of peripheral arthritis in patients with ankylosing spondylitis. Evidence for the development of intestinal inflammation and dysbacteriosis of varying extent of severity in patients with ankylosing spondylitis is supported by research findings. Cold exposure and spine injury may also trigger the disease.
Pathogenesis. Pathogenesis of ankylosing spondylitis has not been well studied. Receptor theory considers antigen as a receptor for damaging factor (for example bacterial antigen, virus, etc.) which causes a disease. Another theory is arthritic peptide theory. According to arthritic peptide theory, an increased immune response to bacterial peptide develops due to combination of peptide with HLA-B27 antigen.
HLA-B27 antigen molecules act as receptors for microbial (for example, Klebsiella pneumonie) and some other triggering factors. The complex which is formed stimulates the production of cytotoxic T-lymphocytes which are able to damage cells and/or tissues having the molecules of this antigen. In HLA-B27-postitive carriers effector CD8+ response which is necessary for elimination of bacteria is decreased, while CD4+ T-cell immunopathologic response is increased.
According to antigen mimicry theory, receptor similarity between HLA-B27 antigen and microbe antigen may contribute to their prolonged persistence in the body of the patient and stimulate the development of an autoimmune process. HLA-B27 peptides do not normally attract T-cells. However, in presence of bacterial peptides which cross-react with them they are typically presented by molecules of the major histocompatibility complex class 2 T-cells and are targeted by T-cell autoimmune attacks.
“Leakage of antigen material” theory, especially of lipopolysaccharides, also exists. Antigen material of lipopolysaccharides usually penetrates through the intestinal wall into the bloodstream due to increased intestinal permeability in patients with ankylosing spondylitis and it is transported to the joints, including sacroiliac joint, cartilages and ligaments.
Pathomorphology. In ankylosing spondylitis “cartilage” joints rather than “synovial” ones are typically involved. They include sacroiliac joints, small intervertebral joints, sternoclavicular and sternocostal joints, symphysis.
Sacroiliitis is a typical early manifestation of ankylosing spondylitis. At the initial stage of the disease granulations which contain lymphocytes, mast cells, macrophages and chondrocytes occur in the subchondral part of the bone. Destruction of cartilage occurs slowly. First articular surfaces are sclerosed. Then fibrous and bone ankylosis of sacroiliac joint typically develops. The articular space usually becomes narrow and ultimately disappears.
Enthesitis, that is inflammation of tendons generally where they attach to bone, ligaments, fibrous part of intervertebral discs and articular capsules, is also typical of ankylosing spondylitis. Inflammation and erosions are typically seen in the foci. In the course of the disease tendons and ligaments are often ossified. Cartilage and fibrous tissue of ligaments and intervertebral discs are most commonly involved. Fibrous tissue of articular capsules of intervertebral joints are less commonly affected.
Spine inflammation and granulation typically occur at the junction of the fibrous ring of the intervertebral disc and vertebral body. External fibers of the fibrous ring are destroyed and replaced by bone tissue which causes formation of bone bridges between vertebrae known as syndesmophytes. Formation of syndesmophytes stops as soon as the intervertebral disc is ossified. The process typically spreads upwards, and radiographic abnormalities of the spine usually resemble a bamboo stick.
Along with these changes, diffuse osteoporosis, inflammation and destruction of vertebral bodies at the junction of the intervertebral disc and square-shaped vertebral bodies are often seen in ankylosing spondylitis. Proliferation of the synovial membrane of intervertebral joints causes destruction of the cartilage of articular processes which sometimes results in bone ankylosis of these joints.
Proliferation of the synovial membrane infiltrated by lymphocytes typically results in peripheral joint involvement. Subchondral granulations and erosions of the cartilage are usually found in the centre of the articular surface. Proliferative synovitis which is less common, may result in pronounced fibrosis of the synovial membrane of the articular capsule. Proliferative synovitis may also predispose to ossification and ankylosis, destruction of the articular cartilage and bone erosions.
Classification.
According to the course of the disease, ankylosing spondylitis may be:
1 Slowly progressive
2 Slowly progressive with exacerbations of the disease
3 Highly progressive (within a short period of time it may lead to complete ankylosis)
4 “Septic” type (it is characterised by an acute onset of the disease, excessive sweating, chills, fever, visceritis, erythrocyte sedimentation rate (ESR) is typically 50 – 60 mm per hour and even more).
The following stages of ankylosing spondylitis are singled out:
The 1st stage is initial or early. It is characterised by moderate limitation of the range of motion of the spine or affected joints; X-ray abnormalities may be absent or may indicate irregular surface of sacroiliac joints, foci of subchondral osteosclerosis, widening of articular spaces.
The 2nd stage is characterised by moderate limitation of the range of motion of the spine or peripheral joints; narrowing or ankylosing of spaces of sacroiliac joints, narrowing of intervertebral articular spaces or signs of ankylosis in spine joints.
The 3rd stage is late. It is characterised by marked limitation of the range of motion of the spine or large joints due to ankylosis; bone ankylosis of sacroiliac joints, intervertebral and costovertebral joints associated with ossification of the ligamentous apparatus.
The following degrees of disease activity are singled out:
 When the cervical part of the spine is involved, the main complaints of the patient are limitation of the range of spine motion and pain when moving the head. The patient cannot touch his breastbone with his chin.
When the cervical part of the spine is involved, the main complaints of the patient are limitation of the range of spine motion and pain when moving the head. The patient cannot touch his breastbone with his chin.
 In some patients pain and stiffness in the loin are often associated with pain in bones. The patient often feels pain in costovertebral and costoclavicular joints, transverse processes of vertebrae, iliac crests, greater trochanters of femurs, ischial tuberosities, tuberosities of shin bones and heel bones. Pain usually aggravates on palpation. Straining and rigidity of paravertebral muscles typically develop as a response to an inflammatory process in the spine. Progressive limitation of the range of spine movements leads to its complete immobility.
The most common and characteristic sites of enthesitis are the insertion of the Achilles tendon on the calcaneus and the insertion of the plantar fascia on the calcaneus.
Hip and shoulder girdle involvement is typical of ankylosing spondylitis. These joints are usually involved over time and in an asymmetric pattern. Hip and shoulder girdle involvement usually results in ankylosis. Other joints, including the joints of lower extremities, may be involved and, if so, in a monooligoarticular pattern. Other peripheral joints are uncommonly involved. Peripheral joint disease occurs in 10 – 15 % of patients.
In about 10% of patients the earliest symptom of ankylosing spondylitis is neuralgia of sciatic nerves characterized by absence of paresthesia and other signs of nerve root involvement as well as by alleviation of pain when moving and aggravation of pain at rest.
Internal organ involvement.
Eye involvement. Anterior uveitis, iritis and iridocyclitis usually occur in 20% of patients. In some patients they may be the first symptoms of ankylosing spondylitis. Sometimes attacks may recur. Iritis (iridocyclitis) is typically seen in patients with ankylosing spondylitis and involvement of peripheral joints. Iritis is usually unilateral, with symptoms of a painful red eye with photophobia and increased lacrimation.
Cardiovascular involvement occurs less commonly, and it is highly variable. Cardiovascular involvement may include aortitis, myocarditis, pericarditis and myocardiodystrophy. Clinical symptoms are usually unclear. Myocarditis is typically associated with atrioventricular block of varying extent.
In ankylosing spondylitis isolated aortic valve insufficiency may be caused by inflammatory changes either in the aorta with its subsequent dilation or in the cusps. Aneurysm of the ascending aorta and the superior part of the descending aorta is likely to occur. Young adults may develop acute aortitis and disorder of the myocardium function. Fibrosis of the subaortic part may cause disorder of impulse conduction and even complete transverse block.
Pulmonary involvement occurs less commonly. Restrictive lung disease may occur in patients with ankylosing spondylitis. Pulmonary emphysema due to kyphosis and costovertebral joint involvement typically develops. Apical pulmonary fibrosis is the most common and characteristic feature of ankylosing spondylitis occurring in 3 – 4% of patients.
Neurologic involvement is rare in ankylosing spondylitis. In some patients signs of peripheral nervous system involvement due to secondary thoracocervical or lumbosacral radiculitis are detected.
In ankylosis and osteoporosis the spine is prone to fractures which can result in spinal injury. Atlantoaxial subluxation and displacement which may result in life- threatening spinal cord or brain stem compression may also occur.
Chronic lumbosacral arachnoiditis (or epiduritis) occurs less commonly. It is often associated with sensitivity and motor disorders as well as dysfunction of pelvic organs. Cauda equina syndrome may also occur in patients with ankylosing spondylitis.
Renal involvement occurs in 5 – 31% of patients with ankylosing spondylitis. Edema, hypertension, anemia and renal insufficiency usually occur at an advanced stage of the disease and are often associated with amyloidosis which is a very common complication of ankylosing spondylitis. Amyloidosis is typically caused by an active inflammatory process and highly progressive course of the disease. Immunoglobulin A (IgA) nephropathy has been also reported in association with ankylosing spondylitis. Urinary syndrome which is clinically manifested by proteinuria and microhematuria may be due to a prolonged administration of nonsteroidal anti-inflammatory drugs which often leads to drug-induced nephropathy.
Gastrointestinal involvement. Asymptomatic inflammation of the colon and ileum has been observed in as many as 50% of patients with ankylosing spondylitis. However, 5 – 10% of patients with established ankylosing spondylitis develop Crohn disease or ulcerative colitis.
Peculiarities of clinical as in males, females and children.
In women exacerbations of the disease alternate with long-lasting remissions. Unilateral sacroiliac joint involvement is more common in females than in males. Women have aortic valve insufficiency more often than men. Men have more severe changes in the spine than women. However, women develop isolated ankylosis of the cervical part of the spine and distal joints of extremites more frequently than men.
In children juvenile ankylosing spondylitis is typically revealed. Children have onset of symptoms before 16 years. The male-to-female ratio is similar to that of adults. It means that ankylosing spondylitis most frequently occurs in males than in females. Juvenile AS is characterised by peripheral arthritis of the joints of lower extremities, especially hip and knee joints as well as by enthesitis. Approximately 1/3 (one third) of children develop acute anterior uveitis. In the course of the disease they complain of pain in the back and sacroilial joints. Peripheral arthritis may disappear or persist. However, hip joint involvement is considered to be a poor prognostic indicator.
Types of clinical course of the disease:
1. Slowly progressive course of the disease is characterised by spine and joint involvement occurring over years. The extent of the disease activity is usually low.
2. Slowly progressive course of the disease with exacerbations is characterised by alternation of remissions with exacerbations leading to disability of the patient.
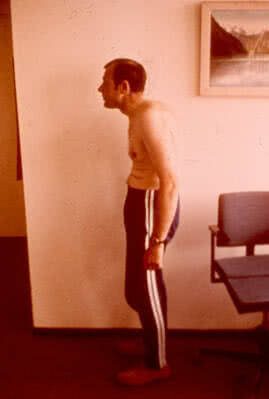
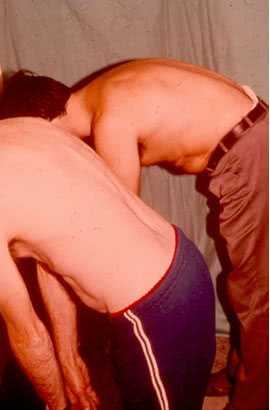
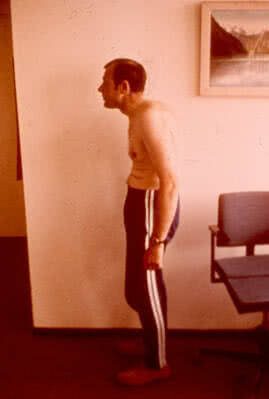
3. Rapidly progressive course of the disease is characterised by pain syndrome, polyarthritis, muscle atrophy, weight loss, elevated indicators of active inflammation, rapid development of kyphosis and ankylosis.
Septic type is characterised by an acute onset of the disease and is often associated with hectic fever, chills, excessive sweating, early signs of internal organ involvement. Septic type makes a definitive diagnosis of AS difficult. In this case ankylosing spondylitis must be differentiated from infectious endocarditis, sepsis and rheumatism. If fever and intoxication are followed by arthritis and stiffness in the spine, the diagnosis of ankylosing spondylitis can be made.
Lab studies. No laboratory tests specific for AS exist. The ESR is elevated in 80% of patients and may not correlate with disease activity. Hypochromic anemia and leukocytosis are rare in ankylosing spondylitis. Other laboratory findings are slightly elevated, but in some patients they remain normal.
In high disease activity the levels of circulating immune complexes and of immunoglobulins A, M and G in the blood serum are elevated.
In peripheral arthritis non-specific inflammatory changes are typically revealed in the synovial fluid. They are the following: neutrophilic leukocytosis, elevated protein level, low viscosity. No ragocytes exist. The complement level is usually normal.
Imaging Studies. In AS sacroiliitis is usually bilateral. Standard radiographs include frontal 25-30° projections in which the sacral bone does not overlap the iliac bone.
The following X-ray stages of sacroileitis are typically singled out:
1) Initial or early stage. The first clinical manifestations of sacroiliitis are considered to be irregular margins of the bone forming the joint, foci of subchondral osteosclerosis and osteoporosis, pseudowidening of the articular space.
2) Stage of moderate injury. Irregular erosions of the margins of the joints, thinning-out of the articular space and pronounced subchondral sclerosis are typical of this stage.
3) Stage of pronounced injury. Periarticular sclerosis associated with formation of bone tissue in the foci of destruction and their partial ankylosis usually occur at this stage. Intervertebral spaces are typically narrowed and signs of ankylosis of true spine joints develop.
4) Late stage. Complete bone ankylosis and obliteration of joints, including sacroiliac, intervertebral and costovertebral with ossification of ligaments are typical of this stage. Sclerosis gradually decreases and leads to the radiographic appearance of osteoporosis at an advanced stage of the disease, and a compact thin line at the site of the sacroiliac joint (the so-called “pseudojoint”).
Imaging studies of spine involvement.
The most common and characteristic feature of ankylosing spondylitis is development of continuous (bridging) syndesmophytes between the adjacent vertebrae. They connect the edges of the upper and lower vertebral bodies. Syndesmophytes develop due to ossification of the peripheral part of intervertebral discs. Most commonly they appear at the junction of thoracic and lumbar vertebrae and are located at the lateral surface of the spine. Less commonly they occur on the anterior surface of the spine and very rarely – on the posterior surface. Over time, development of continuous syndesmophytes may result in a bamboo spine.
In some patients pain and stiffness in the loin are often associated with pain in bones. The patient often feels pain in costovertebral and costoclavicular joints, transverse processes of vertebrae, iliac crests, greater trochanters of femurs, ischial tuberosities, tuberosities of shin bones and heel bones. Pain usually aggravates on palpation. Straining and rigidity of paravertebral muscles typically develop as a response to an inflammatory process in the spine. Progressive limitation of the range of spine movements leads to its complete immobility.
The most common and characteristic sites of enthesitis are the insertion of the Achilles tendon on the calcaneus and the insertion of the plantar fascia on the calcaneus.
Hip and shoulder girdle involvement is typical of ankylosing spondylitis. These joints are usually involved over time and in an asymmetric pattern. Hip and shoulder girdle involvement usually results in ankylosis. Other joints, including the joints of lower extremities, may be involved and, if so, in a monooligoarticular pattern. Other peripheral joints are uncommonly involved. Peripheral joint disease occurs in 10 – 15 % of patients.
In about 10% of patients the earliest symptom of ankylosing spondylitis is neuralgia of sciatic nerves characterized by absence of paresthesia and other signs of nerve root involvement as well as by alleviation of pain when moving and aggravation of pain at rest.
Internal organ involvement.
Eye involvement. Anterior uveitis, iritis and iridocyclitis usually occur in 20% of patients. In some patients they may be the first symptoms of ankylosing spondylitis. Sometimes attacks may recur. Iritis (iridocyclitis) is typically seen in patients with ankylosing spondylitis and involvement of peripheral joints. Iritis is usually unilateral, with symptoms of a painful red eye with photophobia and increased lacrimation.
Cardiovascular involvement occurs less commonly, and it is highly variable. Cardiovascular involvement may include aortitis, myocarditis, pericarditis and myocardiodystrophy. Clinical symptoms are usually unclear. Myocarditis is typically associated with atrioventricular block of varying extent.
In ankylosing spondylitis isolated aortic valve insufficiency may be caused by inflammatory changes either in the aorta with its subsequent dilation or in the cusps. Aneurysm of the ascending aorta and the superior part of the descending aorta is likely to occur. Young adults may develop acute aortitis and disorder of the myocardium function. Fibrosis of the subaortic part may cause disorder of impulse conduction and even complete transverse block.
Pulmonary involvement occurs less commonly. Restrictive lung disease may occur in patients with ankylosing spondylitis. Pulmonary emphysema due to kyphosis and costovertebral joint involvement typically develops. Apical pulmonary fibrosis is the most common and characteristic feature of ankylosing spondylitis occurring in 3 – 4% of patients.
Neurologic involvement is rare in ankylosing spondylitis. In some patients signs of peripheral nervous system involvement due to secondary thoracocervical or lumbosacral radiculitis are detected.
In ankylosis and osteoporosis the spine is prone to fractures which can result in spinal injury. Atlantoaxial subluxation and displacement which may result in life- threatening spinal cord or brain stem compression may also occur.
Chronic lumbosacral arachnoiditis (or epiduritis) occurs less commonly. It is often associated with sensitivity and motor disorders as well as dysfunction of pelvic organs. Cauda equina syndrome may also occur in patients with ankylosing spondylitis.
Renal involvement occurs in 5 – 31% of patients with ankylosing spondylitis. Edema, hypertension, anemia and renal insufficiency usually occur at an advanced stage of the disease and are often associated with amyloidosis which is a very common complication of ankylosing spondylitis. Amyloidosis is typically caused by an active inflammatory process and highly progressive course of the disease. Immunoglobulin A (IgA) nephropathy has been also reported in association with ankylosing spondylitis. Urinary syndrome which is clinically manifested by proteinuria and microhematuria may be due to a prolonged administration of nonsteroidal anti-inflammatory drugs which often leads to drug-induced nephropathy.
Gastrointestinal involvement. Asymptomatic inflammation of the colon and ileum has been observed in as many as 50% of patients with ankylosing spondylitis. However, 5 – 10% of patients with established ankylosing spondylitis develop Crohn disease or ulcerative colitis.
Peculiarities of clinical as in males, females and children.
In women exacerbations of the disease alternate with long-lasting remissions. Unilateral sacroiliac joint involvement is more common in females than in males. Women have aortic valve insufficiency more often than men. Men have more severe changes in the spine than women. However, women develop isolated ankylosis of the cervical part of the spine and distal joints of extremites more frequently than men.
In children juvenile ankylosing spondylitis is typically revealed. Children have onset of symptoms before 16 years. The male-to-female ratio is similar to that of adults. It means that ankylosing spondylitis most frequently occurs in males than in females. Juvenile AS is characterised by peripheral arthritis of the joints of lower extremities, especially hip and knee joints as well as by enthesitis. Approximately 1/3 (one third) of children develop acute anterior uveitis. In the course of the disease they complain of pain in the back and sacroilial joints. Peripheral arthritis may disappear or persist. However, hip joint involvement is considered to be a poor prognostic indicator.
Types of clinical course of the disease:
1. Slowly progressive course of the disease is characterised by spine and joint involvement occurring over years. The extent of the disease activity is usually low.
2. Slowly progressive course of the disease with exacerbations is characterised by alternation of remissions with exacerbations leading to disability of the patient.
3. Rapidly progressive course of the disease is characterised by pain syndrome, polyarthritis, muscle atrophy, weight loss, elevated indicators of active inflammation, rapid development of kyphosis and ankylosis.
Septic type is characterised by an acute onset of the disease and is often associated with hectic fever, chills, excessive sweating, early signs of internal organ involvement. Septic type makes a definitive diagnosis of AS difficult. In this case ankylosing spondylitis must be differentiated from infectious endocarditis, sepsis and rheumatism. If fever and intoxication are followed by arthritis and stiffness in the spine, the diagnosis of ankylosing spondylitis can be made.
Lab studies. No laboratory tests specific for AS exist. The ESR is elevated in 80% of patients and may not correlate with disease activity. Hypochromic anemia and leukocytosis are rare in ankylosing spondylitis. Other laboratory findings are slightly elevated, but in some patients they remain normal.
In high disease activity the levels of circulating immune complexes and of immunoglobulins A, M and G in the blood serum are elevated.
In peripheral arthritis non-specific inflammatory changes are typically revealed in the synovial fluid. They are the following: neutrophilic leukocytosis, elevated protein level, low viscosity. No ragocytes exist. The complement level is usually normal.
Imaging Studies. In AS sacroiliitis is usually bilateral. Standard radiographs include frontal 25-30° projections in which the sacral bone does not overlap the iliac bone.
The following X-ray stages of sacroileitis are typically singled out:
1) Initial or early stage. The first clinical manifestations of sacroiliitis are considered to be irregular margins of the bone forming the joint, foci of subchondral osteosclerosis and osteoporosis, pseudowidening of the articular space.
2) Stage of moderate injury. Irregular erosions of the margins of the joints, thinning-out of the articular space and pronounced subchondral sclerosis are typical of this stage.
3) Stage of pronounced injury. Periarticular sclerosis associated with formation of bone tissue in the foci of destruction and their partial ankylosis usually occur at this stage. Intervertebral spaces are typically narrowed and signs of ankylosis of true spine joints develop.
4) Late stage. Complete bone ankylosis and obliteration of joints, including sacroiliac, intervertebral and costovertebral with ossification of ligaments are typical of this stage. Sclerosis gradually decreases and leads to the radiographic appearance of osteoporosis at an advanced stage of the disease, and a compact thin line at the site of the sacroiliac joint (the so-called “pseudojoint”).
Imaging studies of spine involvement.
The most common and characteristic feature of ankylosing spondylitis is development of continuous (bridging) syndesmophytes between the adjacent vertebrae. They connect the edges of the upper and lower vertebral bodies. Syndesmophytes develop due to ossification of the peripheral part of intervertebral discs. Most commonly they appear at the junction of thoracic and lumbar vertebrae and are located at the lateral surface of the spine. Less commonly they occur on the anterior surface of the spine and very rarely – on the posterior surface. Over time, development of continuous syndesmophytes may result in a bamboo spine.
 At an advanced stage of the disease diffuse osteoporosis of vertebral bodies typically develops.
Radiographic signs of anterior spondylitis should be also considered. Destructive changes of the upper and lower parts of the anterior surface of vertebrae typically lead to loss of the normal concave contour of the anterior surface of the vertebral bodies. Radiographic signs include squaring of the vertebral bodies.
Intervertebral joint involvement associated with the development of ankylosis develop at an advanced stage of the disease. Lumbar part of the spine is usually the first to be involved. Thoracic part is the second to be involved and the cervical part of the spine is the third to be involved. These changes are better seen on oblique radiographs rather than on lateral ones. Sometimes ossification of ligaments of the spine is seen (especially of posterior longitudinal ligament and interosseous ligament).
Changes of peripheral synovial joints.
Standard radiographs usually reveal two types of changes. They are the following:
1) Ossification of the articular capsule, osteosclerosis, osteophytes, ankylosis of joints (most commonly – ankylosis of hip joints).
2) Erosive arthritis with involvement of foot joints, including metatarsophalangeal and interphalangeal joints, big toes.
Enthesitis may develop radiographic changes, including foci of destruction at the sites of insertion of tendons on the spinal processes, crests of the iliac bone, ischial tuberosities, trochanters of femurs, knee-cap, clavicle and, especially on the calcaneus (for example, achillodynitis, plantar fasciitis).
Diagnosis.
Modified New-York criteria (1984) are widely used for diagnosing ankylosing spondylitis. They are the following:
At an advanced stage of the disease diffuse osteoporosis of vertebral bodies typically develops.
Radiographic signs of anterior spondylitis should be also considered. Destructive changes of the upper and lower parts of the anterior surface of vertebrae typically lead to loss of the normal concave contour of the anterior surface of the vertebral bodies. Radiographic signs include squaring of the vertebral bodies.
Intervertebral joint involvement associated with the development of ankylosis develop at an advanced stage of the disease. Lumbar part of the spine is usually the first to be involved. Thoracic part is the second to be involved and the cervical part of the spine is the third to be involved. These changes are better seen on oblique radiographs rather than on lateral ones. Sometimes ossification of ligaments of the spine is seen (especially of posterior longitudinal ligament and interosseous ligament).
Changes of peripheral synovial joints.
Standard radiographs usually reveal two types of changes. They are the following:
1) Ossification of the articular capsule, osteosclerosis, osteophytes, ankylosis of joints (most commonly – ankylosis of hip joints).
2) Erosive arthritis with involvement of foot joints, including metatarsophalangeal and interphalangeal joints, big toes.
Enthesitis may develop radiographic changes, including foci of destruction at the sites of insertion of tendons on the spinal processes, crests of the iliac bone, ischial tuberosities, trochanters of femurs, knee-cap, clavicle and, especially on the calcaneus (for example, achillodynitis, plantar fasciitis).
Diagnosis.
Modified New-York criteria (1984) are widely used for diagnosing ankylosing spondylitis. They are the following:



- Minimum (It is characterised by slight stiffness and pain in the spine and joints of extremities in the morning; ESR is usually 20 mm per hour, C-reactive protein (CRP) +).
- Moderate (It is characterised by persistent pain in the spine and joints, morning stiffness usually lasts for some hours, erythrocyte sedimentation rate is 40 mm per hour, C-reactive protein ++).
- Severe (It is characterised by severe persistent pain in the spine and joints; joint stiffness typically lasts all day long; exudative changes in joints, subfebrile body temperature, visceral manifestations are often seen; ESR is more than 40 mm per hour, C-reactive protein +++).
 When the cervical part of the spine is involved, the main complaints of the patient are limitation of the range of spine motion and pain when moving the head. The patient cannot touch his breastbone with his chin.
When the cervical part of the spine is involved, the main complaints of the patient are limitation of the range of spine motion and pain when moving the head. The patient cannot touch his breastbone with his chin.
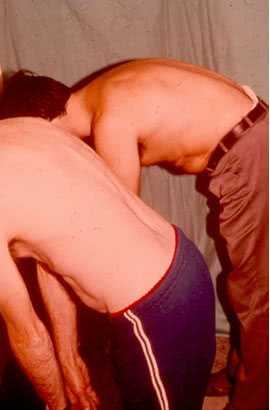 In some patients pain and stiffness in the loin are often associated with pain in bones. The patient often feels pain in costovertebral and costoclavicular joints, transverse processes of vertebrae, iliac crests, greater trochanters of femurs, ischial tuberosities, tuberosities of shin bones and heel bones. Pain usually aggravates on palpation. Straining and rigidity of paravertebral muscles typically develop as a response to an inflammatory process in the spine. Progressive limitation of the range of spine movements leads to its complete immobility.
The most common and characteristic sites of enthesitis are the insertion of the Achilles tendon on the calcaneus and the insertion of the plantar fascia on the calcaneus.
Hip and shoulder girdle involvement is typical of ankylosing spondylitis. These joints are usually involved over time and in an asymmetric pattern. Hip and shoulder girdle involvement usually results in ankylosis. Other joints, including the joints of lower extremities, may be involved and, if so, in a monooligoarticular pattern. Other peripheral joints are uncommonly involved. Peripheral joint disease occurs in 10 – 15 % of patients.
In about 10% of patients the earliest symptom of ankylosing spondylitis is neuralgia of sciatic nerves characterized by absence of paresthesia and other signs of nerve root involvement as well as by alleviation of pain when moving and aggravation of pain at rest.
Internal organ involvement.
Eye involvement. Anterior uveitis, iritis and iridocyclitis usually occur in 20% of patients. In some patients they may be the first symptoms of ankylosing spondylitis. Sometimes attacks may recur. Iritis (iridocyclitis) is typically seen in patients with ankylosing spondylitis and involvement of peripheral joints. Iritis is usually unilateral, with symptoms of a painful red eye with photophobia and increased lacrimation.
Cardiovascular involvement occurs less commonly, and it is highly variable. Cardiovascular involvement may include aortitis, myocarditis, pericarditis and myocardiodystrophy. Clinical symptoms are usually unclear. Myocarditis is typically associated with atrioventricular block of varying extent.
In ankylosing spondylitis isolated aortic valve insufficiency may be caused by inflammatory changes either in the aorta with its subsequent dilation or in the cusps. Aneurysm of the ascending aorta and the superior part of the descending aorta is likely to occur. Young adults may develop acute aortitis and disorder of the myocardium function. Fibrosis of the subaortic part may cause disorder of impulse conduction and even complete transverse block.
Pulmonary involvement occurs less commonly. Restrictive lung disease may occur in patients with ankylosing spondylitis. Pulmonary emphysema due to kyphosis and costovertebral joint involvement typically develops. Apical pulmonary fibrosis is the most common and characteristic feature of ankylosing spondylitis occurring in 3 – 4% of patients.
Neurologic involvement is rare in ankylosing spondylitis. In some patients signs of peripheral nervous system involvement due to secondary thoracocervical or lumbosacral radiculitis are detected.
In ankylosis and osteoporosis the spine is prone to fractures which can result in spinal injury. Atlantoaxial subluxation and displacement which may result in life- threatening spinal cord or brain stem compression may also occur.
Chronic lumbosacral arachnoiditis (or epiduritis) occurs less commonly. It is often associated with sensitivity and motor disorders as well as dysfunction of pelvic organs. Cauda equina syndrome may also occur in patients with ankylosing spondylitis.
Renal involvement occurs in 5 – 31% of patients with ankylosing spondylitis. Edema, hypertension, anemia and renal insufficiency usually occur at an advanced stage of the disease and are often associated with amyloidosis which is a very common complication of ankylosing spondylitis. Amyloidosis is typically caused by an active inflammatory process and highly progressive course of the disease. Immunoglobulin A (IgA) nephropathy has been also reported in association with ankylosing spondylitis. Urinary syndrome which is clinically manifested by proteinuria and microhematuria may be due to a prolonged administration of nonsteroidal anti-inflammatory drugs which often leads to drug-induced nephropathy.
Gastrointestinal involvement. Asymptomatic inflammation of the colon and ileum has been observed in as many as 50% of patients with ankylosing spondylitis. However, 5 – 10% of patients with established ankylosing spondylitis develop Crohn disease or ulcerative colitis.
Peculiarities of clinical as in males, females and children.
In women exacerbations of the disease alternate with long-lasting remissions. Unilateral sacroiliac joint involvement is more common in females than in males. Women have aortic valve insufficiency more often than men. Men have more severe changes in the spine than women. However, women develop isolated ankylosis of the cervical part of the spine and distal joints of extremites more frequently than men.
In children juvenile ankylosing spondylitis is typically revealed. Children have onset of symptoms before 16 years. The male-to-female ratio is similar to that of adults. It means that ankylosing spondylitis most frequently occurs in males than in females. Juvenile AS is characterised by peripheral arthritis of the joints of lower extremities, especially hip and knee joints as well as by enthesitis. Approximately 1/3 (one third) of children develop acute anterior uveitis. In the course of the disease they complain of pain in the back and sacroilial joints. Peripheral arthritis may disappear or persist. However, hip joint involvement is considered to be a poor prognostic indicator.
Types of clinical course of the disease:
1. Slowly progressive course of the disease is characterised by spine and joint involvement occurring over years. The extent of the disease activity is usually low.
2. Slowly progressive course of the disease with exacerbations is characterised by alternation of remissions with exacerbations leading to disability of the patient.
3. Rapidly progressive course of the disease is characterised by pain syndrome, polyarthritis, muscle atrophy, weight loss, elevated indicators of active inflammation, rapid development of kyphosis and ankylosis.
Septic type is characterised by an acute onset of the disease and is often associated with hectic fever, chills, excessive sweating, early signs of internal organ involvement. Septic type makes a definitive diagnosis of AS difficult. In this case ankylosing spondylitis must be differentiated from infectious endocarditis, sepsis and rheumatism. If fever and intoxication are followed by arthritis and stiffness in the spine, the diagnosis of ankylosing spondylitis can be made.
Lab studies. No laboratory tests specific for AS exist. The ESR is elevated in 80% of patients and may not correlate with disease activity. Hypochromic anemia and leukocytosis are rare in ankylosing spondylitis. Other laboratory findings are slightly elevated, but in some patients they remain normal.
In high disease activity the levels of circulating immune complexes and of immunoglobulins A, M and G in the blood serum are elevated.
In peripheral arthritis non-specific inflammatory changes are typically revealed in the synovial fluid. They are the following: neutrophilic leukocytosis, elevated protein level, low viscosity. No ragocytes exist. The complement level is usually normal.
Imaging Studies. In AS sacroiliitis is usually bilateral. Standard radiographs include frontal 25-30° projections in which the sacral bone does not overlap the iliac bone.
The following X-ray stages of sacroileitis are typically singled out:
1) Initial or early stage. The first clinical manifestations of sacroiliitis are considered to be irregular margins of the bone forming the joint, foci of subchondral osteosclerosis and osteoporosis, pseudowidening of the articular space.
2) Stage of moderate injury. Irregular erosions of the margins of the joints, thinning-out of the articular space and pronounced subchondral sclerosis are typical of this stage.
3) Stage of pronounced injury. Periarticular sclerosis associated with formation of bone tissue in the foci of destruction and their partial ankylosis usually occur at this stage. Intervertebral spaces are typically narrowed and signs of ankylosis of true spine joints develop.
4) Late stage. Complete bone ankylosis and obliteration of joints, including sacroiliac, intervertebral and costovertebral with ossification of ligaments are typical of this stage. Sclerosis gradually decreases and leads to the radiographic appearance of osteoporosis at an advanced stage of the disease, and a compact thin line at the site of the sacroiliac joint (the so-called “pseudojoint”).
Imaging studies of spine involvement.
The most common and characteristic feature of ankylosing spondylitis is development of continuous (bridging) syndesmophytes between the adjacent vertebrae. They connect the edges of the upper and lower vertebral bodies. Syndesmophytes develop due to ossification of the peripheral part of intervertebral discs. Most commonly they appear at the junction of thoracic and lumbar vertebrae and are located at the lateral surface of the spine. Less commonly they occur on the anterior surface of the spine and very rarely – on the posterior surface. Over time, development of continuous syndesmophytes may result in a bamboo spine.
In some patients pain and stiffness in the loin are often associated with pain in bones. The patient often feels pain in costovertebral and costoclavicular joints, transverse processes of vertebrae, iliac crests, greater trochanters of femurs, ischial tuberosities, tuberosities of shin bones and heel bones. Pain usually aggravates on palpation. Straining and rigidity of paravertebral muscles typically develop as a response to an inflammatory process in the spine. Progressive limitation of the range of spine movements leads to its complete immobility.
The most common and characteristic sites of enthesitis are the insertion of the Achilles tendon on the calcaneus and the insertion of the plantar fascia on the calcaneus.
Hip and shoulder girdle involvement is typical of ankylosing spondylitis. These joints are usually involved over time and in an asymmetric pattern. Hip and shoulder girdle involvement usually results in ankylosis. Other joints, including the joints of lower extremities, may be involved and, if so, in a monooligoarticular pattern. Other peripheral joints are uncommonly involved. Peripheral joint disease occurs in 10 – 15 % of patients.
In about 10% of patients the earliest symptom of ankylosing spondylitis is neuralgia of sciatic nerves characterized by absence of paresthesia and other signs of nerve root involvement as well as by alleviation of pain when moving and aggravation of pain at rest.
Internal organ involvement.
Eye involvement. Anterior uveitis, iritis and iridocyclitis usually occur in 20% of patients. In some patients they may be the first symptoms of ankylosing spondylitis. Sometimes attacks may recur. Iritis (iridocyclitis) is typically seen in patients with ankylosing spondylitis and involvement of peripheral joints. Iritis is usually unilateral, with symptoms of a painful red eye with photophobia and increased lacrimation.
Cardiovascular involvement occurs less commonly, and it is highly variable. Cardiovascular involvement may include aortitis, myocarditis, pericarditis and myocardiodystrophy. Clinical symptoms are usually unclear. Myocarditis is typically associated with atrioventricular block of varying extent.
In ankylosing spondylitis isolated aortic valve insufficiency may be caused by inflammatory changes either in the aorta with its subsequent dilation or in the cusps. Aneurysm of the ascending aorta and the superior part of the descending aorta is likely to occur. Young adults may develop acute aortitis and disorder of the myocardium function. Fibrosis of the subaortic part may cause disorder of impulse conduction and even complete transverse block.
Pulmonary involvement occurs less commonly. Restrictive lung disease may occur in patients with ankylosing spondylitis. Pulmonary emphysema due to kyphosis and costovertebral joint involvement typically develops. Apical pulmonary fibrosis is the most common and characteristic feature of ankylosing spondylitis occurring in 3 – 4% of patients.
Neurologic involvement is rare in ankylosing spondylitis. In some patients signs of peripheral nervous system involvement due to secondary thoracocervical or lumbosacral radiculitis are detected.
In ankylosis and osteoporosis the spine is prone to fractures which can result in spinal injury. Atlantoaxial subluxation and displacement which may result in life- threatening spinal cord or brain stem compression may also occur.
Chronic lumbosacral arachnoiditis (or epiduritis) occurs less commonly. It is often associated with sensitivity and motor disorders as well as dysfunction of pelvic organs. Cauda equina syndrome may also occur in patients with ankylosing spondylitis.
Renal involvement occurs in 5 – 31% of patients with ankylosing spondylitis. Edema, hypertension, anemia and renal insufficiency usually occur at an advanced stage of the disease and are often associated with amyloidosis which is a very common complication of ankylosing spondylitis. Amyloidosis is typically caused by an active inflammatory process and highly progressive course of the disease. Immunoglobulin A (IgA) nephropathy has been also reported in association with ankylosing spondylitis. Urinary syndrome which is clinically manifested by proteinuria and microhematuria may be due to a prolonged administration of nonsteroidal anti-inflammatory drugs which often leads to drug-induced nephropathy.
Gastrointestinal involvement. Asymptomatic inflammation of the colon and ileum has been observed in as many as 50% of patients with ankylosing spondylitis. However, 5 – 10% of patients with established ankylosing spondylitis develop Crohn disease or ulcerative colitis.
Peculiarities of clinical as in males, females and children.
In women exacerbations of the disease alternate with long-lasting remissions. Unilateral sacroiliac joint involvement is more common in females than in males. Women have aortic valve insufficiency more often than men. Men have more severe changes in the spine than women. However, women develop isolated ankylosis of the cervical part of the spine and distal joints of extremites more frequently than men.
In children juvenile ankylosing spondylitis is typically revealed. Children have onset of symptoms before 16 years. The male-to-female ratio is similar to that of adults. It means that ankylosing spondylitis most frequently occurs in males than in females. Juvenile AS is characterised by peripheral arthritis of the joints of lower extremities, especially hip and knee joints as well as by enthesitis. Approximately 1/3 (one third) of children develop acute anterior uveitis. In the course of the disease they complain of pain in the back and sacroilial joints. Peripheral arthritis may disappear or persist. However, hip joint involvement is considered to be a poor prognostic indicator.
Types of clinical course of the disease:
1. Slowly progressive course of the disease is characterised by spine and joint involvement occurring over years. The extent of the disease activity is usually low.
2. Slowly progressive course of the disease with exacerbations is characterised by alternation of remissions with exacerbations leading to disability of the patient.
3. Rapidly progressive course of the disease is characterised by pain syndrome, polyarthritis, muscle atrophy, weight loss, elevated indicators of active inflammation, rapid development of kyphosis and ankylosis.
Septic type is characterised by an acute onset of the disease and is often associated with hectic fever, chills, excessive sweating, early signs of internal organ involvement. Septic type makes a definitive diagnosis of AS difficult. In this case ankylosing spondylitis must be differentiated from infectious endocarditis, sepsis and rheumatism. If fever and intoxication are followed by arthritis and stiffness in the spine, the diagnosis of ankylosing spondylitis can be made.
Lab studies. No laboratory tests specific for AS exist. The ESR is elevated in 80% of patients and may not correlate with disease activity. Hypochromic anemia and leukocytosis are rare in ankylosing spondylitis. Other laboratory findings are slightly elevated, but in some patients they remain normal.
In high disease activity the levels of circulating immune complexes and of immunoglobulins A, M and G in the blood serum are elevated.
In peripheral arthritis non-specific inflammatory changes are typically revealed in the synovial fluid. They are the following: neutrophilic leukocytosis, elevated protein level, low viscosity. No ragocytes exist. The complement level is usually normal.
Imaging Studies. In AS sacroiliitis is usually bilateral. Standard radiographs include frontal 25-30° projections in which the sacral bone does not overlap the iliac bone.
The following X-ray stages of sacroileitis are typically singled out:
1) Initial or early stage. The first clinical manifestations of sacroiliitis are considered to be irregular margins of the bone forming the joint, foci of subchondral osteosclerosis and osteoporosis, pseudowidening of the articular space.
2) Stage of moderate injury. Irregular erosions of the margins of the joints, thinning-out of the articular space and pronounced subchondral sclerosis are typical of this stage.
3) Stage of pronounced injury. Periarticular sclerosis associated with formation of bone tissue in the foci of destruction and their partial ankylosis usually occur at this stage. Intervertebral spaces are typically narrowed and signs of ankylosis of true spine joints develop.
4) Late stage. Complete bone ankylosis and obliteration of joints, including sacroiliac, intervertebral and costovertebral with ossification of ligaments are typical of this stage. Sclerosis gradually decreases and leads to the radiographic appearance of osteoporosis at an advanced stage of the disease, and a compact thin line at the site of the sacroiliac joint (the so-called “pseudojoint”).
Imaging studies of spine involvement.
The most common and characteristic feature of ankylosing spondylitis is development of continuous (bridging) syndesmophytes between the adjacent vertebrae. They connect the edges of the upper and lower vertebral bodies. Syndesmophytes develop due to ossification of the peripheral part of intervertebral discs. Most commonly they appear at the junction of thoracic and lumbar vertebrae and are located at the lateral surface of the spine. Less commonly they occur on the anterior surface of the spine and very rarely – on the posterior surface. Over time, development of continuous syndesmophytes may result in a bamboo spine.
 At an advanced stage of the disease diffuse osteoporosis of vertebral bodies typically develops.
Radiographic signs of anterior spondylitis should be also considered. Destructive changes of the upper and lower parts of the anterior surface of vertebrae typically lead to loss of the normal concave contour of the anterior surface of the vertebral bodies. Radiographic signs include squaring of the vertebral bodies.
Intervertebral joint involvement associated with the development of ankylosis develop at an advanced stage of the disease. Lumbar part of the spine is usually the first to be involved. Thoracic part is the second to be involved and the cervical part of the spine is the third to be involved. These changes are better seen on oblique radiographs rather than on lateral ones. Sometimes ossification of ligaments of the spine is seen (especially of posterior longitudinal ligament and interosseous ligament).
Changes of peripheral synovial joints.
Standard radiographs usually reveal two types of changes. They are the following:
1) Ossification of the articular capsule, osteosclerosis, osteophytes, ankylosis of joints (most commonly – ankylosis of hip joints).
2) Erosive arthritis with involvement of foot joints, including metatarsophalangeal and interphalangeal joints, big toes.
Enthesitis may develop radiographic changes, including foci of destruction at the sites of insertion of tendons on the spinal processes, crests of the iliac bone, ischial tuberosities, trochanters of femurs, knee-cap, clavicle and, especially on the calcaneus (for example, achillodynitis, plantar fasciitis).
Diagnosis.
Modified New-York criteria (1984) are widely used for diagnosing ankylosing spondylitis. They are the following:
At an advanced stage of the disease diffuse osteoporosis of vertebral bodies typically develops.
Radiographic signs of anterior spondylitis should be also considered. Destructive changes of the upper and lower parts of the anterior surface of vertebrae typically lead to loss of the normal concave contour of the anterior surface of the vertebral bodies. Radiographic signs include squaring of the vertebral bodies.
Intervertebral joint involvement associated with the development of ankylosis develop at an advanced stage of the disease. Lumbar part of the spine is usually the first to be involved. Thoracic part is the second to be involved and the cervical part of the spine is the third to be involved. These changes are better seen on oblique radiographs rather than on lateral ones. Sometimes ossification of ligaments of the spine is seen (especially of posterior longitudinal ligament and interosseous ligament).
Changes of peripheral synovial joints.
Standard radiographs usually reveal two types of changes. They are the following:
1) Ossification of the articular capsule, osteosclerosis, osteophytes, ankylosis of joints (most commonly – ankylosis of hip joints).
2) Erosive arthritis with involvement of foot joints, including metatarsophalangeal and interphalangeal joints, big toes.
Enthesitis may develop radiographic changes, including foci of destruction at the sites of insertion of tendons on the spinal processes, crests of the iliac bone, ischial tuberosities, trochanters of femurs, knee-cap, clavicle and, especially on the calcaneus (for example, achillodynitis, plantar fasciitis).
Diagnosis.
Modified New-York criteria (1984) are widely used for diagnosing ankylosing spondylitis. They are the following:
- Low back pain with inflammatory characteristics
- Limitation of lumbar spine motion in sagittal and frontal planes
- Osteochondrosis of the spine
- Rheumatoid arthritis (especially in peripheral joint involvement)