Дополнительные материалы к обновленным (2017г) рекомендациям по лечению спондилоартритов, включая анкилозирующие спондилиты и псориатические артриты, до достижения цели
Supplementary Material A
A systematic literature review to inform the task force on “Treating spondyloarthritis, including ankylosing spondylitis and psoriatic arthritis, to target: 2017 update of recommendations by an international task force”
The systematic literature review was performed by Monika Schöls
Дополнительная таблица S1. Термины поиска в базе данных Medline
| (((((((spondylarthr*[Title]) OR spondyloarthr*[Title]) OR ankylosing[Title]) OR (axial[Title] AND SpA[Title])) OR (radiologic*[Title] AND SpA[Title])) OR (radiographic*[Title] AND SpA[Title])) OR Bechterew[Title]) OR (psoria*[Title] AND arthr*[Title]) |
Дополнительная таблица S2. Исследовательские вопросы для систематического поиска литературы, которые были сформулированы целевой группой, в том числе по обновлению поиска T2T испытаний против обычного лечения 2011-2016
В1. Ремиссия лучшая цель, чем LDA в отношении исхода?
В2. Что является лучшим определением цели? (т. е. какая цель наиболее тесно связана с результатами, определенными в вопросе Q1?)
Q3. Следует ли использовать визуализацию и лабораторию (включая биомаркеры) в дополнение к клинической оценке для мониторинга заболеваний?
В4. Каковы потенциальные риски T2T? Связано ли большее количество лекарств и ранняя эскалация с большим количеством AE (краткосрочная и долгосрочная) и / или более высокой стоимостью? Является ли концепция T2T экономически эффективной?
В5. Существуют ли пациентские и сопутствующие факторы, влияющие на вероятность достижения цели?
В6. Ранняя ремиссия приводит к лучшему результату?
Q7. Как долго после начала приема нового препарата вы должны подождать, прежде чем можете решить, что препарат неэффективен?
В8. Реагируют ли спинальные и периферические проявления аналогично или по-разному?
В9. Будет ли результат лучше, если пациенты понимают концепцию T2T?
T2T=treat to target; LDA=low disease activity, низкая активность болезни; AE=adverse event, побочная реакция.
| Q1. Is remission a better target than LDA with respect to outcome? |
| Q2. What is the best target definition? (i.e., which target is related most closely to the outcomes defined in Q1?) |
| Q3. Should imaging and lab (including biomarkers) be used in addition to clinical assessment to monitor disease? |
| Q4. What are potential risks of T2T? Are more drugs and early escalation related to more AE (short and long-term), and / or higher costs? Is the concept of T2T cost-effective? |
| Q5. Are there patient and contextual factors that affect the likelihood to achieve a target? |
| Q6. Is earlier remission leading to a better outcome? |
| Q7. How long after start of a new drug should you wait before you can decide that the drug is inefficacious? |
| Q8. Do spinal and peripheral involvements respond similarly or differently? |
| Q9. Is the outcome better if patients understand the T2T concept? |
T2T=treat to target; LDA=low disease activity; AE=adverse events.
Дополнительная Table S3. Определение результата исследования.
Определение результата для СпА и ПсА
- Участия в общественной жизни, в том числе трудоспособности
- Физические возможности
- Качество жизни
- Структурное повреждение
- Коморбидности (сердечно-сосудистые заболевания / риском сердечно-сосудистых заболеваний)
- Токсичность
- Смертность
- Внесуставных проявлений
| Outcome definition for SpA and PsA |
| Social participation including work capacity |
| Physical function |
| Quality of life |
| Structural damage |
| Comorbidity (cardiovascular disease / CV risk) |
| Toxicity |
| Mortality |
| Extra-articular manifestations |
Q1. Is remission a better target than LDA with respect to outcome?
Нет исследований отвечающих на этот вопрос.
Существует, однако, одно исследование, которое доказывает концепцию T2T: исследование TICOPA сравнивает целевое лечение и стандартную помощь пациентам с псориатическим артритом:
TICOPA исследование о Т2Т при раннем ПсА (1)
- открытое многоцентровое РКИ, П=206 (101 T2T)
- ранний (менее 2-х лет длительность симптомов), DMARD -наивный ПсА
- тест сжатия кисти (TC) tight control (TC) arm: посещение каждые 4 недели; при каждом посещении оценивались критерии MDA
- DMARDs использовались по максимуму. доза согласно протоколу, если pts ( [Protocol Type Selection] правила выбора протокола) не достиг MDA.
- Компаратор: стандартное лечение (СЛ) standard care (SC) руки: общая ревматология амбулаторная клиника; контроль каждые 12 недель (чаще, если необходимо); нет формальных проявлений активности заболевания, нет требования или ограничения по назначению
- open-label multicentre RCT, N=206 (101 T2T)
- early (less than 2 years symptom duration), DMARD-naïve PsA
- tight control (TC) arm: visit every 4 weeks; at each visit, MDA criteria were assessed
- DMARDs were escalated to the max. dose according to protocol if pts. had not achieved MDA.
- comparator: standard care (SC) arm: general rheumatology outpatient clinic; reviewed every 12 weeks (more often if indicated); no formal measures of disease activity, no requirement or restriction on prescribing
Первичный результат: исходы по
ACR20 в 48 недель:
- Шансы достижения ответа ACR20 в течение 48 недель были выше по сравнению с стандартным лечением после направления в центр и уточнения артрита (OR 1,91, 95% CI 1,03-3,55, p=0,0392).
- Более высокая доля пациентов с тестом сжатия (55/89 (61,8%)) достигла ответа ACR20 за 48 недель по сравнению с пациентами с стандартным лечением (37/84 (44,0%)
- ACR50 (OR: 2.36, 1.25, 4.47, р=0·0081) и ACR70 (OR: 2.64, 1.32, 5.26, р=0·0058) в течение 48 недель были выше при тесте сжатия по сравнению с стандартной терапией.
- Небольшое увеличение доли при pts. При эрозивной болезни для обоих TX(treatment) рук (30.7%); JSN оставалась подобной той, что наблюдается на базовых (85.8%). Общей Медиана в модификации Sharp-van der Heijde scores (mvdHS)баллы (mvdHS) на 48 неделе остались похожие на TX (лечение) рук (8.0 TC против 6.0 СК). Никаких доказательств различия в изменениях в mvdHS баллы, кстати (между прочим) btw. TX рук на 48 неделе (p=0·9779), со средней сменой нуля в обеих руках.
- PROs: Pts in TC отмечалась более высокая медиана улучшения в PsAQoL (3.0 TC и 0.5 СК). Большую долю в ТЦ удовлетворяют пороговому MCID изменения в результат HAQ от BL(basal), базальный до 48 неделю (58.2% TC против 41.1% СК)
TICOPA AE/SAE and CEA смотри ниже
Primary outcome: proportion of
ACR20 at 48 weeks:
- odds of achieving ACR20 response at 48 weeks were higher in TC arm compared to the SC arm after adjusting for centre and arthritis classification (OR91, 95% CI 1.03-3.55, p=0.0392).
- higher proportion of TC patients (55/89 (61.8%)) achieved an ACR20 response at 48 weeks compared to SC patients (37/84 (44.0%)
- ACR50 (OR: 2.36, 1.25, 4.47, p=0·0081) and ACR70 (OR: 2.64, 1.32, 5.26, p=0·0058) at 48 weeks were higher in the TC arm compared to the SC
- slight increase in the proportion of with erosive disease for both TX arms (30.7%); JSN remained similar to that observed at baseline (85.8%). Median total modified Sharp-van der Heijde scores (mvdHS) at week 48 remained similar across TX arms (8.0 TC vs 6.0 SC). No evidence of a difference in the change in mvdHS scores btw. TX arms at week 48 (p=0·9779), with median change of zero in both arms.
- PROs: Pts in TC reported greater median improvement in PsAQoL (3.0 TC vs. 0.5 SC). Greater proportion in TC met the MCID threshold for the change in HAQ score from BL to week 48 (58.2% TC vs 41.1% SC)
TICOPA AE/SAE and CEA see below
Q2. What is the best target definition? (i.e., which target is related most closely to the outcomes defined in Q1?)
Дополнительная Таблица S4. Изученные связи между целями и результатами (2011-2016)
Supplementary Table S4. Investigated associations between targets and outcomes (2011-2016)
Псориатические артриты
|
TARGET |
OUTCOME |
RESULTS |
| Psoriatic Arthritis |
| Comparison btw. MDA-targeted tight control (TC) and standard care (SC) |
| Coates 2016(2) TICOPA |
MDA |
Radio: mSvdH Score |
slight increase in the proportion of pts with erosive disease for both TX arms (30.7%); JSN similar to baseline (85.8%). Median total mvdHS scores at w 48 remained similar across TX arms (8.0 TC vs 6.0 SC). No evidence of a difference in the change in mvdHS scores btw. TX arms at w 48 (p=0·9779); median change of zero in both arms. |
| Association studies between targets and outcomes |
| Kavanaugh 2015(3;4) |
DAS28-REM <2.6* |
Work: workplace and household productivity: validated arthritis-specific Work Productivity Survey (WPS). |
sign. better productivity outcomes in short-term DAS28-REM achievers |
| Kavanaugh 2013(5) |
DAS28-CRP |
Work: daily productivity at work, school, or home in the previous 4 weeks (self- reported VAS)
Function: HAQ
QoL: SF-36 PCS |
Week 52 DAS28-CRP REM achievers:
SF-36 PCS>50: OR 8.4 (p< 0.0001)
SF-36 MCS>50: OR 2.0; p<0.01
Week 104 DAS28-CRP REM achievers:
SF-36 PCS>50: OR 9.9 (p< 0.0001)
SF-36 MCS>50: OR 2.5 (p<0.001) |
| Coates 2016(6) |
MDA |
QoL |
Greater improvements in SF-36 MCS and PCS, PsAQoL were seen among MDA responders compared to non-responders at weeks 24 and 52 |
| Coates 2015(2) |
MDA |
Radio: total SvdH score |
Achieving MDA sign. predictive of total SvdH score for median and some 75/90th quantile scores: radiographic progression consistently numerically lower in those achieving MDA. |
| Kavanaugh 2016(7) |
MDA |
Radio: mean change from BL in SHS |
Irrespective of TX, MDA at ≥3 and ≥4 consecutive visits was associated with sign. less radiographic progression |
| Cheng 2016(8) |
MDA |
CVD: subclinical atherosclerosis evaluated by carotid intima-media thickness (IMT) at BL, 12 and 24 months |
At 12 months, mean carotid IMT sign. lower in sustained sMDA group than non-sMDA group [0.612±0.049mm vs 0.668±0.130mm (p=0.030)]; no signif. changes in the maximum IMT. Baseline mean carotid IMT associated with month 12 mean carotid IMT (p<0.001). ANCOVA: adjusted mean carotid IMT remained significantly lower in the sMDA group (0.612±0.023 mm vs 0.666±0.012 mm resp., p=0.041) after adjusting for BL mean carotid IMT. Signif. difference in change in mean IMT (-0.01± 0.08mm in sMDA group, vs 0.05± 0.08mm in non-sMDA group, p=0.046). Differences were statistically insignificant after adjusting for BL differences probably due to small number. No significant changes were observed in the change in maximum IMT. |
| Aletaha 2017(9) |
DAPSA |
Function: HAQ
QoL: SF-36-PCS
Radio: PsA-mSvdH-Score |
6-months HAQ and DAPSA: p<0.0001 between REM, LDA, mod. DA, HDA at 6 m
6-months SF-36 PCS and DAPSA: p<0.0001 between REM, LDA, mod. DA, HDA at 6 m |
| Eder 2015(10) |
DAPSA |
CVD: vascular ultrasound of the carotid arteries; total plaque area: extent of atherosclerosis |
association btw. inflammation over time and atherosclerosis assessed by regression models adjusted for age, sex and CV risk factors à DAPSA (p=0.04) associated with more severe atherosclerosis. (not significant after adjustment for traditional CVD risk factors) |
| Simon 2012(11) |
SJC
TJC, CRP, ESR |
Radio: Ratingen score of hands and feet |
Progressive radiological damage during 12 months FU more frequent with increasing SJC (8 of 26 visits; 30.8%) than with stable or decreased number of SJ (5 of 89 visits; 5.6%; p=0.001). |
| Axial SpA |
| Association studies between targets and outcomes
|
| van der Heijde 2016(12) |
ASDAS: inactive disease state<1.3 |
Work: Productivity and Activity Impairment Questionnaire;
Function: HAQ;
QoL: SF-36 PCS |
Pts. grouped by clinical response (ASAS40 response and ASDAS states at w12). Changes in PROs BL to w12 compared btw. groups using analysis of covariance with adjustment for BL scores.
ASAS40 responders sign. greater improvement in mean HAQ-S (-0.65 vs -0.05, P<0.0001), SF-36 PCS (12.4 vs 0.7, P<0.0001), presenteeism (-24.7 vs -2.2, P<0.0001), overall work impairment (-23.9 vs -2.5, P<0.0001) and activity impairment (-33.5 vs -0.9, P<0.0001) at week 12 vs. non-resp.
ASDAS-ID: achievers had a mean HAQ-S of 0.26 corresp. to normal function and a mean SF-36 PCS of 47.9 corresp. To normal function. à normal function in ASDAS-ID 61.5% vs. non-ID 14.7, p<0.0001)
Similar in ASDAS clinically important improvement and major improvement: assoc. with sign. greater improvements from BL. |
| van Lunteren 2016(13;14) |
ASDAS |
Work: Work Productivity Loss (WPL), Presenteeism, absenteeism in the past 7 days. |
1-point increase in ASDAS resulted in an increase of 18.5%, 16.9%, 9.6% in WPL, presenteeism and absenteeism, respectively. |
| Machado 2011(15) |
ASDAS
BASDAI |
Function: BASFI
HRQoL: SF-36 PCS, MCS |
SF-36 PCS associated with physical function and disease activity (adjusted R(2) (adjR(2))=0.39-0.40). SF-36 MCS independently associated with physical function (adjR(2)=0.07). Physical function was independently associated with measures of spinal mobility and disease activity (adjR(2)=0.39-0.45). Spinal mobility was hierarchically shown to be an intermediate variable btw. structural damage and physical function, while physical function was shown to be intermediate btw. spinal mobility and the physical component of SF-36. HRQoL is determined by physical function and disease activity, physical function is determined by spinal mobility and disease activity, and spinal mobility is determined by structural damage and inflammation of the spine. |
| van Lunteren 2016(16) |
ASDAS |
QoL: SF-36 PCS |
decrease in disease activity assoc. with clear improvement in QoL: decrease of one unit of ASDAS BL to 1y resulted in improvement in PCS of 9.2 (SE 1.6) over 1y. Fulfilment of the clinical or imaging arm (p=0.036) and gender (p=0.082) were effect modifiers in the model for PCS. |
| Ramiro 2014(17) |
ASDAS
BASDAI
CRP |
Radio: mSASSS |
models with ASDAS fitted the data better than models with BASDAI, CRP or BASDAI+CRP. An increase of one ASDAS unit led to an increase of 0.72 mSASSS units/2 yrs. A ‘very high disease activity’ (ASDAS >3.5) compared with ‘inactive disease’ (ASDAS <1.3) resulted in an additional 2-y. progression of 2.31 mSASSS units. The effect of ASDAS on mSASSS was higher in males vs. females (0.98 vs -0.06 mSASSS units per ASDAS unit) and in pts. with <18yrs. vs ≥18yrs. symptom duration (0.84 vs 0.16 mSASSS units per ASDAS unit). CONCL.: 1st study showing that disease activity contributes longitudinally to radiographic progression in the spine in AS. effect more pronounced in men and in earlier disease. |
| Poddubnyy 2016(18) |
Time-averaged ASDAS
CRP
BASDAI
PtGA |
Radio: mSASSS; Syndesmophyte formation/progression |
clear positive association: logistic regression analysis: mSASSS progression by ≥2 points over 2 yrs. sign. assoc. with time-averaged ASDAS: unadjusted OR=1.64 (95% CI 1.03 to 2.62), adjusted (for presence of syndesmophytes at baseline, smoking status and NSAIDS) OR=1.80 (95% CI 1.04 to 3.13). Syndesmophyte formation/progression demonstrated an even stronger association with the time-averaged ASDAS: unadjusted OR=2.62 (95% CI 1.46 to 4.68), adjusted OR=2.45 (95% CI 1.26 to 4.77).
trend for positive association btw. single components of the ASDAS (BASDAI, CRP and PtGA) and mSASSS worsening by two points and stat sign. assoc. btw. syndesmophyte formation/progression and CRP (OR 1.07; 1.01–1.13) as well as PtGA (OR 1.30; 1.01–1.69) |
| Fongen 2013(19) |
ASDAS HDA |
Function: International PA Questionnaire; weekly energy expenditure; proportion reaching health enhancing physical activity (HEPA). |
HDA sign. lower total weekly energy expenditure (MET) than LDA (p=0.02, p=0.01, resp.) and lower amounts of walking (p<0.01, p=0.02, resp.) and vigorous activity (p=0.06, p=0.06, resp.). Only 41% with HDA reached HEPA vs. 61% in LDA (p=0.02). HDA: lower weekly energy expenditure in PA than LDA and less likely to reach HEPA than LDA. |
| Castillo-Ortiz 2016(20) |
BASDAI
BASFI |
Work: standardized Work Disability (WD) rates; reduction in working hours |
BL predictors of adverse work outcome over 12 yrs.: worse BASFI (HR 1.2 [95% CI 1.0, 1.4]).
Time-varying predictors over 12 yrs.: BASFI, BASDAI (WD already prevalent at inclusion, a substantial proportion of pts. incurred further adverse work outcome over 12 yrs. In addition to country of residence, uveitis, age, and self-reported physical function or disease activity predicted long-term adverse work outcome.) |
| Fabreguet 2012(21) |
PGA
BASDAI |
Work instability: AS-WIS; patients with low work instability (AS-WIS < 11) vs. moderate to high WI |
mean AS-WIS score was 9.5 (5.5); 55 (35%) pts. had moderate and 8 (5%) pts. had high work instability. Correlations of the AS-WIS score with SpA scores significant but moderate (BASDAI R = 0.42, BASFI R = 0.41, PGA R = 0.53; P < 0.0001). In multivariate analysis, high PGA was the only element associated with moderate to high WIS. |
| Chen 2015(22) |
APR |
Function: BASFI
physical mobility: BASMI |
ESR mildly correlated with BASFI (r=0.176, p=0.028) and moderately correlated with BASMI (r=0.427, p<0.001). CRP moderately correlated with BASMI (r=0.410, p<0.001).
ROC: ESR, CRP, and disease duration showed best AUC in distinguishing pts. with poor physical mobility (BASMI≥3.6, the Median) (AUC=0.748, 0.751 and 0.738, resp., all p<0.001), as compared to BASDAI, BASFI, and BASG. ESR×disease duration (AUC=0.801, p<0.001) and CRP × disease duration (AUC=0.821, p<0.001) showed higher AUC values than ESR or CRP alone in indicating poor physical mobility. For detecting poor physical mobility (BASMI≥3.6). ESR×disease duration (≥60.0mm/h×y.): sensitivity=72.7 % and specificity=72.8 %; CRP×disease duration (≥8.3mg/dl×y.): sensitivity=72.7 % and specificity=74.6%. ESR, CRP, and disease duration are particularly related to AS pt.’s poor physical mobility |
| Laatiris 2012(23) |
Enthesitis: Mander Enthesis Index (MEI);
Maastricht AS Enthesitis Score (MASES) |
QoL: SF-36 |
Severity of enthesitis sign. correlated with disease activity, functional disability and degradation of quality of life. |
| Wick 2012(24) |
Time averaged CRP |
Radio: SPARCC semi-quant. assessment: annual progression of erosions in sacroiliac MRI |
time-averaged CRP (CRP; mg/l), /AUC. The mean (SD) CRP decreased from 1.3 (1.8) at BL to 0.5 (0.6) at FU MRI (p<0.04), which has been performed after a mean (SD) disease course of 2.8 (1.5) yrs. The mean (SD) annual increase (∆) of SPARCC score from BL to FU MRI was 0.4 (0.4). BL individual SPARCC sub-score for bone marrow edema did not statistically sign. correlate with individual ∆SPARCC sub-score for erosions (p=N.S.). The individual AS pt. correlation btw. annual time-averaged CRP and each annual ∆SPARCC sub-scores was only statistically significant for erosions (p<0.01; r =0.71). |
| Konsta 2016(25) |
Time averaged CRP |
Radio: mSASSS |
time-averaged CRP >5mg/L is an independent risk factor for spinal radiographic progression during TNFi (OR: 6.4, CI: 1.9-21) |
| Berg 2015(26) |
APR
ASDAS |
CVD: elevated arterial stiffness (augmentation index); pulse wave velocity (PWV)) |
Increasing BL values of CRP, ESR and ASDAS associated with elevated AIx on FU (p(trend) 0.01, 0.05 and 0.04, resp.). Similar non-significant patterns for PWV. In the multivariate analyses, BL CRP and ASDAS were independently associated with future elevated AIx (p=0.03 and 0.02, resp.). In multivariate PWV model, results for CRP and ASDAS non-significant. |
| Bakland 2011(27) |
CRP |
Mortality |
crude mortality among AS pts. 14.5% (98 pts.); Standardised Mortality Rate was only sign. increased among male vs. female pts. (1.63 vs 1.38, p<0.001). Factors independently associated with reduced survival were diagnostic delay (OR 1.05), increasing levels of CRP (OR 2.68), work disability (OR 3.65) and not using NSAIDs (OR 4.35). |
DAS28=Disease Activity Score28 Счет активности болезни 28; REM=remission ремиссия РЕМ*, РМС*; DAPSA=Disease Activity in PSoriatic Arthritis Score; MDA=Minimal disease activity минимальная активность болезни МАБ*; SJC=swollen joint count счет опухших суставов; TJC=tender joint count счет болезненных суставов; CRP=C-reactive protein; ESR=erythrocyte sedimentation rate; APR=acute phase reactants; ASDAS=Ankylosing Spondylitis Disease Activity Score; BASDAI=Bath Ankylosing Spondylitis Disease Activity Index; BASFI=Bath Ankylosing Spondylitis Functional Index; PGA=physician global assessment глобальная врачебная оценка; REM=remission; PGA=physician global assessment глобальная врачебная оценка;; modDA=moderate disease activity умеренная(средняя) активность болезни УАБ*, САБ* ; HDA=high disease activity высокая активность болезни ВАБ*; PtGA=patient global assessment глобальная оценка пациентом; HAQ=health assessment questionnaire; mSvdH score=modified Sharp-van der Heijde score; VAS=visual analogue scale визуальная аналоговая шкала ВАШ; QoL=quality of life качество КЖ*; HRQoL=Health related quality of life качество жизни связанное со здоровьем; SF-36 PCS=short Form-36 questionnaire; PCS physical component score; MCS=mental component score; mSASSS=modified Stoke Ankylosing Spondylitis Spinal Score; SPARCC=Spondyloarthritis Research Consortium of Canada Index; CVD=cardiovascular disease; BL=baseline. *presumably DAS28ESR, but not indicated in the paper.
- Русская аббревиатура, предложено автором
DAS28=Disease Activity Score 28; REM=remission; DAPSA=Disease Activity in PSoriatic Arthritis Score; MDA=Minimal disease activity; SJC=swollen joint count; TJC=tender joint count; CRP=C-reactive protein; ESR=erythrocyte sedimentation rate; APR=acute phase reactants; ASDAS=Ankylosing Spondylitis Disease Activity Score; BASDAI=Bath Ankylosing Spondylitis Disease Activity Index; BASFI=Bath Ankylosing Spondylitis Functional Index; PGA=physician global assessment; REM=remission; LDA=low disease activity; modDA=moderate disease activity; HDA=high disease activity; PtGA=patient global assessment; HAQ=health assessment questionnaire; mSvdH score=modified Sharp-van der Heijde score; VAS=visual analogue scale; QoL=quality of life; HRQoL=Health related quality of life; SF-36 PCS=short Form-36 questionnaire; PCS physical; component score; MCS=mental component score; mSASSS=modified Stoke Ankylosing Spondylitis Spinal Score; SPARCC=Spondyloarthritis Research Consortium of Canada Index; CVD=cardiovascular disease; BL=baseline. *presumably DAS28ESR, but not indicated in the paper.
Q3. Should imaging and lab (including biomarkers) be used in addition to clinical assessment to monitor disease?
При АС, есть доказательства, что индексом basdai+СРБ имеют лучшее отношение к mSASSS, чем в одиночку индексом BASDAпо данным анализа данных когорты OASIS. (17)
Информация о комбинированной визуализации и клинической оценке отсутствует.
In AS, there is evidence that BASDAI
+CRP have a better relationship to mSASSS than BASDAI alone according to analyses of OASIS cohort data.(17)
There is no information on combined imaging and clinical assessment.
Q4. What are potential risks of T2T? Are more drugs and early escalation related to more adverse events (short and long-term), and / or higher costs? Is the concept of T2T cost-effective?
According to results of the TICOPA study,(1)
- adverse events (AE) were reported more commonly in the tight control (TC) arm (97.0%, n=98) vs. standard care (SC) arm (77.1%, n=81).
- in pts. experiencing an event, a higher median number of AE were reported in TC (6.0 (range: 1.0, 20.0)) vs. SC (3.0; range 1.0-10.0).
- most commonly reported: nausea (10.6%), liver abnormalities (8.8%), and infections (common cold) (6.9%).
- serious adverse events (SAE) were reported more common in TC arm (including those suspected to be related to trial medications):
- 25 SAE observed in 14 pts. (13.9%) vs. 8 SAE observed in 6 pts. (5.7%) in SC.
- 10 SAE were suspected to be related to drug therapy, with 8 in the TC arm (cellulitis (n=2), pneumonia (n=2), musculosceletal chest pain (n=1), raised liver function tests (n=1), collapse and pancytopenia (n=1), anaphylaxis (n=1)) and 2 in the SC arm (migraine, septic arthritis).
- TC is unlikely to be considered cost-effective using willingness to pay thresholds of £20,000 to £30,000 per QALY.
ТС
вряд ли будет считаться экономически эффективным, используя готовность платить предельно от £20 000 до 30 000 фунтов на QALY
Q5. Are there patient and contextual factors that affect the likelihood to achieve a target?
Дополнительная таблица S5. Пациент и конституциональные факторы
Supplementary Table S5. Patient and contextual factors
| |
Study |
Type |
N |
factor |
TARGET |
TX |
FU |
|
| Smoking |
| PsA |
Hojgaard 2015(28) |
Observationalcohort study; DANBIO registry. |
1388 |
smoking status (current CU/never NE/ previous PRE) |
ACR20/50/70-responses EULAR-good-response |
1st TNFi |
6 m |
CU vs. NE:
- EULAR-good-response (23% vs. 34% p<0.05)
- ACR20 (24% vs. 33% p<0.05)
ACR50 (17% vs. 24% p<0.05), most pronounced in men. |
| axial SpA |
Glintborg 2016(29) |
Observational cohort study: Danish nationwide DANBIO registry
axSpa |
1576 |
smoking status |
BASDAI 50%/20 mm- response |
1st TNFi |
6 m |
CU vs. NE
- BASDAI50%/20 mm-response rate 42%/58%, P<0.001
- BASDAI50%/20 mm-response OR 0.48 (0.35-0.65), P<0.0001: CU lower odds
|
| Ciurea 2016(30) |
Swiss Clinical Quality Management Cohort
axSpA |
698 |
smoking status |
BASDAI and ASDAS binary response rates at 1y |
1st TNFi |
1 y |
CU vs. NE:
- smaller reductions in BASDAI upon TX (0.75 units less, p=0.005) for pts. with elevated BL CRP level
- smaller reductions in ASDAS upon TX (0.69 units less, 0.001) for pts. with elevated BL CRP level
- Odds for BASDAI50% improvem. after 1y sign. lower (0.54, 0.31-0.95, p=0.03)
- Odds for ASAS40% after 1y sign. lower (0.43, 0.24-0.76, p=0.004)
|
| Obesity |
| PsA |
Di Minno 2011(31) |
PsA |
135 |
BMI: 1st degree (BMI <30) and 2nd degree (BMI 30-35 ) obesity |
MDA |
TNFi |
24 mths |
Obesity associated with higher risk of not achieving MDA (HR 4.90, 3.04-7.87; P<0.001). HR of not achieving MDA: 3.98 (1.96-8.06, P<0.001) and 5.40 (3.09-9.43, P<0.001) in subjects with 1st degree and 2nd degree obesity, resp.
Among subjects who achieved MDA at 12-mths, presence of obesity was associated with a poor probability of sustained MDA at 24-mths. FU (HR 2.04, 1.015-3.61; P=0.014). |
| Iannone 2013(32) |
Retrospective
PsA |
135 |
BMI |
DAS28-REM
SDAI-REM |
TNFi |
36 m |
BMI did not predict REM or changes in HAQ following TNFi:
DAS28-REM (37%) or SDAI-REM (21%) of obese not sign. different from overweight and normal weight pts. (44% and 21%, resp.). |
| Di Minno 2014(33) |
Prospective
PsA |
138 |
weight loss /
dietary intervention |
MDA |
TNFi |
6 m |
≥5% of weight loss after 6 mths. TNFi, was a predictor of the achievement of MDA (OR=4.20, 95% CI 1.82 to 9.66, p<0.001). For increasing weight-loss categories (<5%, 5-10%, >10%), MDA was achieved by 23.1%, 44.8% and 59.5%, resp. Higher rate of MDA achievement in pts. with 5-10% (OR=3.75, 95% CI 1.36 to 10.36, p=0.011) and in those with >10% (OR=6.67, 2.41 to 18.41, p<0.001) weight loss vs. those with <5% weight loss. |
| Eder 2015(34) |
PsA |
577 |
BMI: normal (<25) overweight (25-30) and obese (>30) |
Sustained MDA: LDA state in ≥5 of following domains for at least 1y.: skin, enthesitis, tender and SJCs, pain, PtGA and function. |
|
FU ≥1y |
dose-response association btw. BMI and probability of sustained MDA in the multivariate regression analysis: Pts. in higher BMI categories less likely to achieve sustained MDA vs. lowest BMI category: overweight: OR 0.66 p=0.003; obese: OR 0.53 p<0.0001) after adjusting for potential confounding variables. |
| Costa 2015(35) |
PsA |
330 |
metabolic syndrome (MetS; identified by NCEP-ACT III) |
MDA |
TNFi |
12 and 24 m |
inverse association btw. presence of MetS and probability of achieving MDA. Univariate analysis: MetS less likely to achieve MDA (OR 0.45, p<0.001); also stat. sign. in multivariate regression (OR 0.56, p<0.001). |
| Iervolino 2012(36) |
PsA |
146 |
MetS and/or liver steatosis |
MDA |
TNFi |
3 m |
prevalence of MetS and liver steatosis showed no significant differences btw. subjects achieving MDA and those who did not (p=0.347 and 0.053, resp.).
ESR: sign. reduction (p<0.001). CRP: no sign. variation (p > 0.05). Pts. achieving MDA at T3 were younger (p =0.001). Lower BL TJC (p=0.001), SJC (p =0.013), BASDAI (p=0.021), and Ritchie index (p=0.006) in pts. achieving MDA. Age (OR 0.896, p=0.003) and BASFI (OR 0.479, p=0.007) inversely predicted, CRP (OR 1.78, p=0.018) directly predicted, MDA at T3. à In pts. with PsA, age, CRP, and BASFI at beginning of TX were reliable predictors of MDA after 3 mths. TNFi. |
| axial SpA |
Gremes 2014(37) |
Retrospective
axSpA |
170 |
BMI and gender
normal weight (BMI<25), overweight (BMI 25-30) and obese
(BMI≥30) |
BASDAI50 primary EP
BASDAI≤1 secondary EP |
TNFi |
12 m |
rate of BASDAI50 achievement 72.8% in normal weight vs. 54.5% in overweight and 30.4% in obese subjects (P<0.001)
best independent predictors of failure to obtain a BASDAI50 response at the 12 m were female gender [OR 3.23 (95% CI 1.52, 7.14)] and BMI ≥ 30 [OR 3.57 (95% CI 1.15, 11.11)]. |
| Ottaviani 2012(38) |
retrospective
axSpA |
155 |
BMI |
BASDAI50, VAS50, CRP50, NSAID use50 – dichotomized with a threshold decrease of 50% of initial level of the measure, into binary variables assessing response to IFX / (log. regr.) |
TNFi |
6 m |
higher BMI associated with lower BASDAI50 (P=0.0003; OR, 0.87 (0.81-0.94)), VAS50 (P<0.0001; OR, 0.87 (0.80-0.93); CRP50 (P=0.0279; OR, 0.93 (0.88-0.99), and NSAID50 (P=0.0077; OR, 0.91 (0.85-0.97). |
| Machado 2011(15) |
axSpA |
214 |
BMI |
SF-36 MCS |
|
|
association in univariate lin. regr.: R2=0.039; p0.004 |
| Gender |
| axial SpA |
van der Horst-Bruinsma 2013(39) |
data pooled from 4 clinical control trials
axSpA |
1283 |
gender |
differences/ similarities in BL demographics, disease
characteristics, and efficacy, safety, discontinuation rates after 12 weeks. |
ETA, SSZ, PLAC |
12 weeks |
Women had sign. (p<0.001) smaller differences in all week 12 efficacy assessments including ASDAS (0.87 vs -1.08), BASDAI (-19.22 vs -23.41) and BASFI (-13.89 vs -16.88) vs. men. Similar relationship btw. women and men in the adjusted mean diff. of nocturnal back pain (4.04, 95% CI 0.77-7.32; p<0.05), total back pain (3.80, 0.77-7.32; p<0.05) and PtGA (4.79, 1.51-8.08; p<0.01). |
| Lorenzin 2015(40) |
Retrospective
axSpA |
70 |
gender |
BASDAI, BASFI, BASMI |
TNFi |
5 y |
Non-responders predominantly females (34.3 % vs 17.1 %). |
| Perrotta FM 2014(41) |
axSpA |
214 |
CRP
Dis dur
ESR
BASMI
BASDAI
BASFI |
Partial REM (pREM; <20mmVAS in each of the 4: PtGA/last week; pain (spinal pain)/ BASFI; inflammation [mean intensity and duration of MST |
TNFi |
12 m |
high CRP≥2 vs ≤0.8 mg/dL were associated with higher rate of pREM; pREM was associated with shorter disease duration ≤36 vs ≥189 mths. and higher ESR ≥45 vs ≤17 mm/h. In male pts. lower BASMI≤2 vs ≥6 and absence of psoriasis were associated with higher pREM rate only at 12 mths. Other parameters assessed before TX, such as BASDAI, BASFI, peripheral arthritis, inflammatory bowel disease and uveitis were not associated with PR. |
| Gremese 2014(37) |
Retrospective
axSpA |
170 |
Gender
BMI |
BASDAI50 primary EP
BASDAI≤1 secondary EP |
TNFi |
12 m |
best independent predictors of failure to obtain a BASDAI50 response at 12 m. were female gender [OR 3.23 (95% CI 1.52, 7.14)] and BMI ≥ 30 [OR 3.57 (95% CI 1.15, 11.11)]. |
| Machado 2011(15) |
axSpA |
214 |
Gender (male) |
QoL: SF-36 PCS |
|
|
association in univariate lin. regr.: R2 0.034, p=0.007 |
| van Lunteren 2016(16) |
axSpA |
|
gender |
QoL |
|
|
decrease in disease activity is associated with a clear improvement in health-related quality of life, but effect higher in men. |
| Others |
| PsA |
Iervolino 2012(36) |
|
146 |
age |
MDA |
TNFi |
3 m |
Pts. achieving MDA at 3 m younger than those not achieving MDA (p =0.001). |
| AS |
Machado 2011(15) |
Stratified model |
214 |
age |
QoL: SF-36 PCS
Function: BASFI |
|
|
association in univariate lin. regr.: age à dependent variable BASFI R2=0.038, p=0.004
association in univariate lin. regr.: age à dependent variable SF-36 PCS R2=0.037; p=0.005 |
CU=current smoker; NE=never smoker; PRE=previous smoker; NON=nonsmoking; PY=pack year; TX=treatment; BASDAI=Bath Ankylosing Spondylitis Disease Activity Index; y=year; ASDAS=Ankylosing Spondylitis Disease Activity Score; ASAS40=Assessment of SpondyloArthritis International Society 40% response; BASFI=Bath Ankylosing Spondylitis Functional Index; ESR=erythrocyte sedimentation rate; CRP=C-reactive protein; mSASSS=modified Stoke Ankylosing Spondylitis Spinal Score; BASFI=Bath Ankylosing Spondylitis Functional Index; ACR20/50/70=American College of Rheumatology 20/50/70% response; BMI=body mass index; EP=endpoint; NSAID=nonsteroidal anti rheumatic drug; MDA=Minimal disease activity; VAS=visual analogue scale; QoL=quality of life; SF-36 PCS=short Form-36 questionnaire; PCS physical; component score; MCS=mental component score; MetS=metabolic syndrome; TNFi=tumor necrosis factor alpha inhibitor; mths=months; ASQoL Ankylosing Spondylitis Quality of Life questionnaire; DAS28=Disease Activity Score 28; REM=remission;, SDAI=simplified disease activity index.
Q6. IS EARLIER REMISSION LEADING TO A BETTER OUTCOME?
нет доказательств
Q7. HOW LONG AFTER START OF A NEW DRUG SHOULD YOU WAIT BEFORE YOU CAN DECIDE THAT THE DRUG IS INEFFICACIOUS?
There is evidence available for a 12-week time point (RAPID- trial data; Certolizumab in axSpA or PsA(42))
- AxSpA: Wk48 ASDAS-ID was achieved by 0% of pts who had ASDAS very high disease activity at Wk12, vs. 68% of pts with ASDAS-ID at Wk12
- PsA: Wk48 MDA was achieved by 0% of pts who had DAS28(CRP)>5.1 at Wk12, vs. 73% of pts with DAS28(CRP)<2.6.
- à Using disease activity and clinical response state during after a maximum of 12 wks of CZP, it was possible to identify a subset of patients unlikely to achieve long-term treatment goals.
Evidence for 6 months’ time point (BioTRAC-registry(43))
PsA patients treated with IFX, N=106
- Among patients with MDA at 6 months, 75.0% had sustained MDA at 12 months, while and among the non- achievers, only 14.8% achieved MDA at 12 months of treatment.
Q8. DO SPINAL AND PERIPHERAL INVOLVEMENTS RESPOND SIMILARLY OR DIFFERENTLY?
нет доказательств
Q9. IS THE OUTCOME BETTER IF PATIENTS UNDERSTAND THE T2T CONCEPT?
нет доказательств
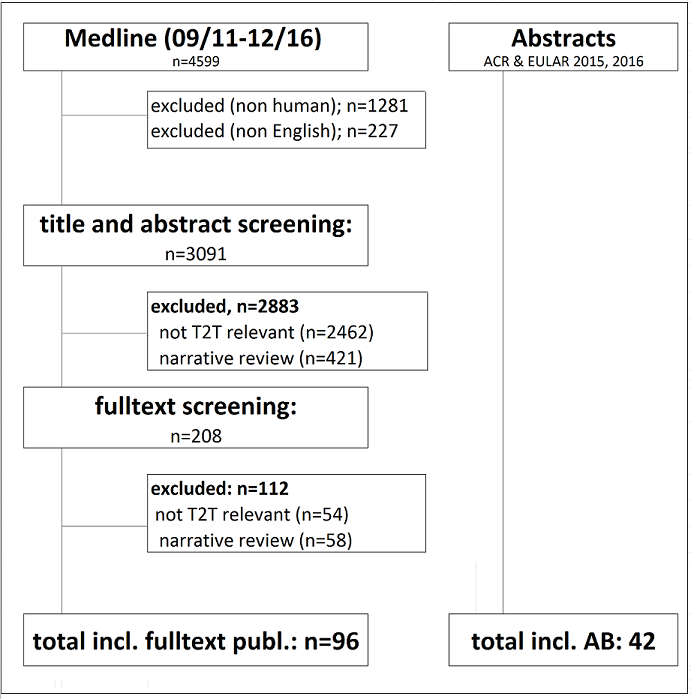
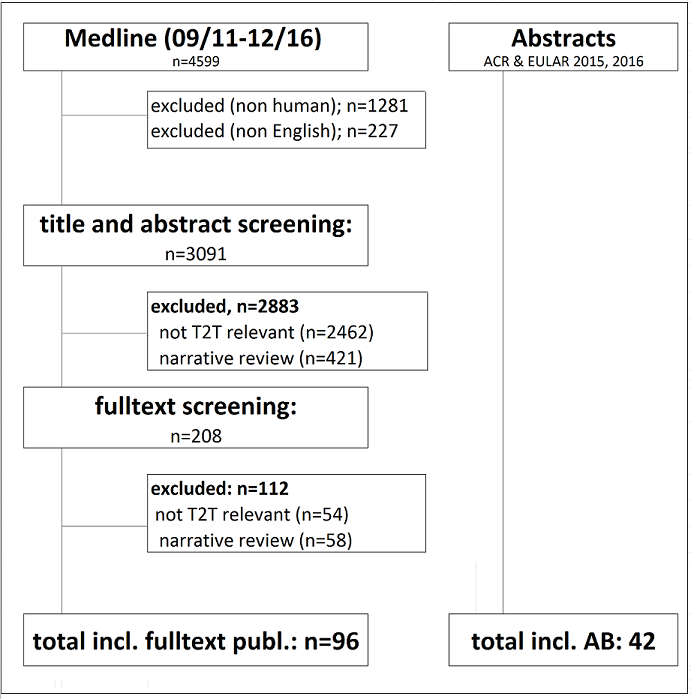
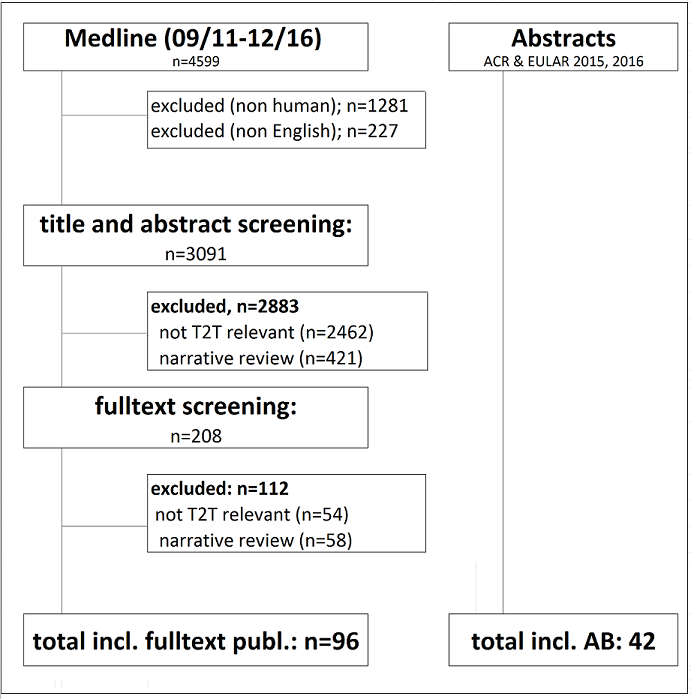
Пояснения для дополнительного рисунка S1. Legend for Supplementary Figure S1.
Figure S1. Диаграмма, иллюстрирующая процесс выбора .Flow Chart Illustrating the Selection Process.
T2T=treat to target; AB=abstract.
ССЫЛКИ
(1) Coates LC, Moverley AR, McParland L, et al. Effect of tight control of inflammation in early psoriatic arthritis (TICOPA): a UK multicentre, open-label, randomised controlled trial. Lancet 2015;386(10012):2489-2498.
(2) Coates LC, Hensor E, Emery P, et al. Does treat to target or achieving remission improve radiographic outcomes in PsA? Arthritis Rheum 2015;68 (Suppl 10).
(3) Kavanaugh A, Gladman D, van der Heijde DM, et al. Clinical responses in joint and skin outcomes and patient reported outcomes are associated with increased productivity in the workplace and at home in psoriatic arthritis patients treated with certolizumab pegol. Arthritis Rheum 2015;67 (Suppl 10).
(4) Kavanaugh A, Gladman D, van der Heijde DM, et al. Clinical Responses in Joint and Skin Outcomes and Patient-Reported Outcomes are Associated with Increased Productivity in the Workplace and at Home in Psoriatic Arthritis Patients Treated with Certolizumab Pegol. Value in Health 2015;18(7):a654.
(5) Kavanaugh A, McInnes I, Krueger G, et al. Patient-reported outcomes and the association with clinical response in patients with active psoriatic arthritis treated with golimumab: findings through 2 years of a phase III, multicenter, randomized, double-blind, placebo-controlled trial. Arthritis Care Res 2013;65(10):1666-1673.
(6) Coates LC, Mease P, Gossec L, et al. Patients with active psoriatic arthritis achieving minimal disease activity with secukinumab treatment demonstrate sustained improvement of function and quality of life. Arthritis Rheum 2016;68 (Suppl 10).
(7) Kavanaugh A, van der Heijde DM, Beutler A, et al. Radiographic Progression of Patients With Psoriatic Arthritis Who Achieve Minimal Disease Activity in Response to Golimumab Therapy: Results Through 5 Years of a Randomized, Placebo-Controlled Study. Arthritis Care Res (Hoboken ) 2016;68(2):267-274.
(8) Cheng TH, Shang Q, Lee PWA, et al. Can achieving sustained minimal disease activity (MDA) prevent progression of subclinical arthrosclerosis? A prospective cohort study in psoriatic arthritis. Arthritis Rheum 2016;68 (Suppl 10).
(9) Aletaha D, Alasti F, Smolen JS. Disease activity states of the DAPSA, a psoriatic arthritis specific instrument, are valid against functional status and structural progression. Ann Rheum Dis 2016;76(2):418-421.
(10) Eder L, Thavaneswaran A, Chandran V, Cook R, Gladman DD. Increased burden of inflammation over time is associated with the extent of atherosclerotic plaques in patients with psoriatic arthritis. Ann Rheum Dis 2015;74(10):1830-1835.
(11) Simon P, Pföhler C, Bergner R, et al. Swollen joint count in psoriatic arthritis is associated with progressive radiological damage in hands and feet. Clin Exp Rheumatol 2012;30:45-50.
(12) van der Heijde DM, Joshi A, Pangan AL, et al. ASAS40 and ASDAS clinical responses in the ABILITY-1 clinical trial translate to meaningful improvements in physical function, health-related quality of life and work productivity in patients with non-radiographic axial spondyloarthritis. Rheumatology 2016;55:80-88.
(13) van Lunteren M, Bakker P, Ez-Zaitouni Z, et al. [THU0409] Is disease activity associated with work productivity loss, presenteeism, and absenteeism in patients with early axial spondyloarthritis? Results from the SPACE cohort. Ann Rheum Dis 2016;75 (Suppl2):336.
(14) van Lunteren M, Bakker P, Ez-Zaitouni Z, et al. Is disease activity associated with work productivity loss, presenteism and absenteism in patients with early axial spondyloarthritis? Results from the Spondyloarthritis Caught Early (SPACE) cohort. Arthritis Rheum 2016;68 (Suppl 10).
(15) Machado P, Landewe R, Braun J, et al. A stratified model for health outcomes in ankylosing spondylitis. Ann Rheum Dis 2011;70:1758-1764.
(16) van Lunteren M, Ez-Zaitouni Z, Bakker P, et al. [THU0383] Does change in disease activity over one year result in change in health-related quality of life in axial spondyloarthritis patients? Ann Rheum Dis 2016;75 (Suppl2):326.
(17) Ramiro S, van der Heijde DM, van Tubergen A, et al. Higher disease activity leads to more structural damage in the spine in ankylosing spondylitis: 12-year longitudinal data from the OASIS cohort. Ann Rheum Dis 2014;73(1455):1461.
(18) Poddubnyy D, Protopopov M, Haibel H, et al. High disease activity according to the Ankylosing Spondylitis Disease Activity Score is associated with accelerated radiographic spinal progression in patients with early axial spondyloarthritis: results from the GErman SPondyloarthritis Inception Cohort. Ann Rheum Dis 2016;75(12):2114-2118.
(19) Fongen C, Halvorsen S, Dagfinrud H. High disease activity is related to low levels of physical activity in patients with ankylosing spondylitis. Clin Rheumatol 2013;32:1719-1725.
(20) Castillo-Ortiz JD, Ramiro S, Landewe R, et al. Work Outcome in Patients With Ankylosing Spondylitis: Results From a 12-Year Followup of an International Study. Arthritis Care Res (Hoboken ) 2016;68(4):544-552.
(21) Fabreguet I, Koumakis E, Burki V, et al. Assessment of work instability in spondyloarthritis: a cross-sectional study using the ankylosing spondylitis work instability scale. Rheumatology 2012;51:333-337.
(22) Chen CH, Chen HA, Liao HT, et al. The clinical usefulness of ESR, CRP, and disease duration in ankylosing spondylitis: the product of these acute-phase reactants and disease duration is associated with patient’s poor physical mobility. Rheumatol Int 2015;35:1263-1267.
(23) Laatiris A, Amine B, Yacoub YI, et al. Enthesitis and its relationships with disease parameters in Moroccan patients with ankylosing spondylitis. Rheumatol Int 2012;32:723-727.
(24) Wick MR, Grundtman C, Weiss RJ, et al. The time-averaged inflammatory disease activity estimates the progression of erosions in MRI of the sacroiliac joints in ankylosing spondylitis. Clin Rheumatol 2012;31(1117):1121.
(25) Konsta M, Sakellariou G, Iliopoulos A, et al. Long-term effect of TNF inhibitors on radiographic progression in ankylosing spondylitis is associated with syndesmophytes at baseline and time-averaged CRP levels. Arthritis Rheum 2016;68 (Suppl 10).
(26) Berg IJ, Semb AG, van der Heijde DM, et al. CRP and ASDAS are associated with future elevated arterial stiffness, a risk marker of cardiovascular disease, in patients with ankylosing spondylitis: results after 5-year follow-up. Ann Rheum Dis 2015;74(8):1562-1566.
(27) Bakland G, Gran JT, Nossent JC. Increased mortality in ankylosing spondylitis is related to disease activity. Ann Rheum Dis 2011;70:1921-1925.
(28) Hojgaard P, Glintborg B, Hetland ML, et al. Association between tobacco smoking and response to tumour necrosis factor á inhibitor treatment in psoriatic arthritis: results from the DANBIO registry. Ann Rheum Dis 2015;74(12):2130-2136.
(29) Glintborg B, Hojgaard P, Hetland ML, et al. Impact of tobacco smoking on response to tumour necrosis factor-alpha inhibitor treatment in patients with ankylosing spondylitis: results from the Danish nationwide DANBIO registry. Rheumatology 2016;55(4):659-668.
(30) Ciurea A, Scherer A, Weber U, et al. Impaired response to treatment with tumour necrosis factor á inhibitors in smokers with axial spondyloarthritis. Ann Rheum Dis 2016;75(3):532-539.
(31) Di Minno A, Peluso R, Iervolino S, et al. Obesity and the prediction of minimal disease activity: a prospective study in psoriatic arthritis. Arthritis Care Res (Hoboken ) 2013;65(1):141-147.
(32) Iannone F, Fanizzi R, Scioscia C, et al. Body mass does not affect the remission of psoriatic arthritis patients on anti-TNF-a therapy. Scand J Rheum 2013;42(1):41-4.
(33) Di Minno MN, Russolillo A, Di Minno A, et al. Weight loss and achievement of minimal disease activity in patients with psoriatic arthritis starting treatment with tumour necrosis factor á blockers. Ann Rheum Dis 2014;73:1157-1162.
(34) Eder L, Thavaneswaran A, Chandran V, et al. Obesity is associated with a lower probability of achieving sustained minimal disease activity state among patients with psoriatic arthritis. Ann Rheum Dis 2015;74(5):813-817.
(35) Costa L, Caso F, Ramonda R, et al. Metabolic syndrome and its relationship with the achievement of minimal disease activity state in psoriatic arthritis patients: an observational study. Immunol Res 2015;61:147-153.
(36) Iervolino S, Di Minno MND, Peluso R, et al. Predictors of early minimal disease activity in patients with psoriatic arthritis treated with tumor necrosis factor-á blockers. J Rheumatol 2012;39:568-573.
(37) Gremese E, Bernardi S, Bonazza S, et al. Body weight, gender and response to TNF-á blockers in axial spondyloarthritis. Rheumatology 2014;53:875-881.
(38) Ottaviani S, Allanore Y, Tubach F, et al. Body mass index influences the response to infliximab in ankylosing spondylitis. Arthritis Res Ther 2012;14(3):R115.
(39) van der Horst-Bruinsma IE, Zack DJ, Szumsi A, et al. Female patients with ankylosing spondylitis: analysis of the impact of gender across treatment studies. Ann Rheum Dis 2013;72:1221-1224.
(40) Lorenzin M, Ortolan A, Frallonardo P, et al. Predictors of response and drug survival in ankylosing spondylitis patients treated with infliximab. BMC Musculoskeletal Disord 2015;16:166.
(41) Perrotta FM, Addimanda O, Ramonda R, et al. Predictive factors for partial remission according to the Ankylosing Spondylitis Assessment Study working group in patients with ankylosing spondylitis treated with anti-TNFá drugs. Reumatismo 2014;66(3):208-214.
(42) van der Heijde DM, Deodhar A, Fleischmann R, et al. Early Disease Activity or Clinical Response Predict Long-Term Outcomes with Certolizumab Pegol in Axial Spondyloarthritis or Psoriatic Arthritis. Arthritis Care Res (Hoboken ) 2016; doi: 10.1002/acr.23092. [Epub ahead of print].
(43) Sholter D, Rahman P, Sheriff M, et al. Disease progression among non-achievers of minimal disease activity in PsA patients treated with infliximab or golimumab. Arthritis Rheum 2016;68 (Suppl 10).
Дополнительные материалы В Supplementary Material B
Для ясности мы не приводим в основной части рукописи все детали обсуждения вокруг отдельных общих принципов или рекомендаций. Для того чтобы все же отразить эти детали, чтобы они не утрачены, особенно в отношении будущих обновлений этих рекомендаций, эти пункты обсуждения представлены здесь.
Основополагающие принципы
- C. Spa и PSA являются многогранными системными заболеваниями; лечение мышечно-скелетных и внесуставные проявлений должно координироваться, по мере необходимости, между ревматологом и другими специалистами (такими как дерматологи, гастроэнтерологи, офтальмологи).
Обсуждены дальнейшие пункты: Spa и PSA вызваны сочетанием генетических, экологических и факторы образа жизни, некоторые из которых еще не были идентифицированы и могут отличаться в зависимости от проявлений болезни; следовательно, “многогранный” было предложено заменить “сложное”. Во-вторых, в качестве незначительного изменения “по мере необходимости” был перенесен в центр с начала второй части этого принципа. Был также обсужден вопрос о том, следует ли заменить” вне-суставной ““extra-articular словом” вне-мышечноскелетным““extra-musculoskeletal”, однако преобладало мнение о том, что выражение”вне-суставной “ всегда понималось как внутренний орган, а не как скелетные (т. е. суставы и связанные с ними структуры) проявления. Некоторые члены целевой группы упомянул – тоже в процесс подготовки рукописи – что для них энтезит был суставной характеристикой; в строгом смысле слова в entheses не являются частью сустава, о чем свидетельствует Leeds Enthesitis Index
1и даже иногда рассматривается как “enthesis organ”;
2, 3 “энтезис как органа”; дактилит, в то время как часто пан-пальцевое pan-digital воспаление, связанное с тендовагинит, которые могут быть иногда даже при отсутствии суставного синовита;
4, 5 и осевое поражение является, как правило, отделенным от периферических суставов. Однако, очевидно, что они являются симптомами заболевания опорно-двигательного аппарата. Поэтому мы называем их “вне-суставные костно-мышечные проявления” “non-articular musculoskeletal manifestations” ради семантической согласованности.
Рекомендации
- Цель лечения должна быть клиническая ремиссия/неактивность заболевания по мышечноскелетным (артрит, дактилит, энтезит, осевая болезнь) и внесуставных проявлениям.
Другие обсуждаемые моменты: Включение этих признаков не означает, что ревматологи должны сосредоточиться на лечении внесуставных (т. е. органных) проявлений, поскольку их могут лечить другие специалисты, в соответствии с всеобъемлющим принципом C. Далее, как упоминалось в 2012 году, “ремиссия” и “неактивное заболевание”“inactive disease” рассматривались как синонимы, поскольку с учетом всеобъемлющего принципа Е, подавление воспаления имеет важное значение и подразумевает возвращения активности заболевания. Важно отметить, что эта рекомендация касается общей темы, а не какой-либо конкретной меры или оценки; эти вопросы рассматриваются в последующих пунктах.
- Цель лечения должна быть индивидуализирована на основе текущих клинических проявлений заболевания; методика лечения должна учитываться при определении времени, необходимого для достижения цели.
Дополнительно обсуждаемые вопросы: в настоящее время до сих пор нет доказательств с точки зрения соответствующих стратегических исследований, что индивидуализация лечения на основании клинических проявлений не имеет никаких преимуществ; впрочем, это предполагалось целевой группой, поскольку, например, значительные поражения кожи в дополнении вовлечения суставов может потребовать различную стратегию в отношении лекарств, при артрите с только маленькие кожные проявления или серьезных заболеваний кожи по низким активности артритом.6, 7 Акцент на индивидууме был более подчеркнут в обновлении рекомендаций Т2Т для РА за 2014 год путем переноса соответствующей рекомендации вверх, с пункта 9 на пункт 5.8 Кроме того, Данные о реальной практике из норвежского регистра DMARD показали, что расхождение между оценкой активности пациента и врача по заболеваниям может снизить вероятность достижения ремиссии как при РА, так и PsA.9
- Клиническая ремиссия / неактивность заболевания определяется как отсутствие клинико-лабораторных данных о значимой активности заболевания.
Обсуждались и другие вопросы: необходимо быть обеспокоенным, если пациент имеет высокий СРБ при отсутствии клинической активности.10 Дополнительный пункт обсуждения, связанный с термином “существенный”“significant”. Однако в ходе обсуждений было решено, что наличие одного остаточного болезнености и/или опухшего сустава или минимальная остаточная аксиальная боли не должны препятствовать, рассматривать пациента как находящемуся в ремиссии. Подобные решения должны применяться к энтезиту и псориазу. Наконец, в предыдущей версии использовался термин “ воспалительная активность заболевания”“inflammatory disease activity”, но поскольку активность при заболеваниях всегда “воспалительна” в нынешнем контексте и воспаление уже рассматривалось в общих принципах, было принято решение простым большинством голосов исключить это прилагательное
- Низкая / минимальная активность заболевания может быть альтернативной целью лечения.
Дополнительные вопросы для обсуждения: Хотя исследование TICOPA показало лучшие клинические, функциональные и качественные результаты жизни при ориентировании на MDA по сравнению с неуправляемым подходом, радиографические изменения, являющиеся важным отдельным результатом, не отличались между группами лечения.11 Это может быть следствием дизайна, при которой обе группы получали активную терапию при ранних заболеваниях, но нельзя исключать, что подход Т2Т не может превосходить обычное лечение по важными конечными точками.
Список литературы
- Healy PJ, Helliwell PS. Measuring clinical enthesitis in psoriatic arthritis: assessment of existing measures and development of an instrument specific to psoriatic arthritis. Arthritis Rheum 2008;59:686-691.
- McGonagle D, Tan AL. The enthesis in psoriatic arthritis. Clin Exp Rheumatol 2015;33(5 Suppl 93):S36-S39.
- Benjamin M, McGonagle D. The enthesis organ concept and its relevance to the spondyloarthropathies. Adv Exp Med Biol 2009;649:57-70.
- Olivieri I, Barozzi L, Favaro L et al. Dactylitis in patients with seronegative spondylarthropathy. Assessment by ultrasonography and magnetic resonance imaging. Arthritis Rheum 1996;39(9):1524-1528.
- Tan AL, Fukuba E, Halliday NA, Tanner SF, Emery P, McGonagle D. High-resolution MRI assessment of dactylitis in psoriatic arthritis shows flexor tendon pulley and sheath-related enthesitis. Ann Rheum Dis 2015;74(1):185-189.
- Coates LC, Kavanaugh A, Mease PJ et al. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2015 Treatment Recommendations for Psoriatic Arthritis. Arthritis Rheumatol 2016;68(5):1060-1071.
- Gossec L, Smolen JS, Ramiro S et al. European League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis 2016;75(3):499-510.
- Smolen JS, Breedveld FC, Burmester GR et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis 2016;75(1):3-15.
- Michelsen B, Kristianslund EK, Hammer HB et al. Discordance between tender and swollen joint count as well as patient’s and evaluator’s global assessment may reduce likelihood of remission in patients with rheumatoid arthritis and psoriatic arthritis: data from the prospective multicentre NOR-DMARD study. Ann Rheum Dis 2016;76(4):708-711.
- Poddubnyy D, Haibel H, Listing J et al. Baseline radiographic damage, elevated acute-phase reactant levels, and cigarette smoking status predict spinal radiographic progression in early axial spondylarthritis. Arthritis Rheum 2012;64(5):1388-1398.
- Coates LC, Moverley AR, McParland L et al. Effect of tight control of inflammation in early psoriatic arthritis (TICOPA): a UK multicentre, open-label, randomised controlled trial. Lancet 2015;386(10012):2489-2498.
Дополнительный материал 1